Understanding Moral Injury in Health Care 13 Jan 5:28 PM (2 months ago)
Physicians for a National Health Program (PNHP) is partnering with the Robert Wood Johnson Foundation (RWJF) to study the impact of financialization on U.S. health care. Starting in the fall of 2024, and continuing through the summer of 2025, we will engage current health care professionals to better understand moral injury and distress, how these issues impact racial inequities in health care, and how best to remedy this worsening problem.
Take our brief moral injury survey
Toolkit: Share our moral injury survey
Dr. Diljeet Singh explains our research project
What is “moral injury?”
As health care has been transformed from an essential service to a profit-driven business, the morale of the entire workforce—including physicians, nurses, and allied health professionals—has suffered. This trend has led to shortages as professionals are retiring early, cutting back work hours, quitting clinical medicine, and tragically committing suicide in increasing numbers.
These responses have often been misdiagnosed as “burnout,” but the lack of efficacy of standard treatments for burnout has led insightful scholars such as Drs. Wendy Dean and Simon Talbot to identify “moral injury” as a more accurate culprit.
Moral injury in health care is described as the challenge of knowing what care patients need, but being unable to provide it due to constraints beyond physicians’ control. As a result, our focus on burnout is insufficient and, in fact, causes harm by leading to a reliance on ineffectual “wellness” programs and an obscuring of root causes. Without adequate data on moral injury, the ability of policymakers and stakeholders to address our health care crisis will remain limited.
Gaps in the literature
In an effort to better understand moral injury in health care, PNHP will survey workers throughout the medical profession and will conduct a series of 20-40 one-on-one interviews with currently practicing physicians. We will gather data points on the impact of financialization from our survey, and identify narratives from our interviews to more compellingly illustrate these data points. These elements will form the basis of our fall 2025 report, which will provide actionable recommendations for stakeholders.
Our project follows the rigorous practices of the Association for the Accreditation of Human Research Protection Programs (AAHRPP), and we have obtained Institutional Review Board approval by the independent Pearl IRB, along with our consultant at Cambridge Health Alliance’s institutional IRB.
See the following documents for specifics on our survey, and the broader moral injury project:
- Grant agreement and expectations from RWJF
- IRB approval letter from Pearl IRB
- IRB approval letter from Cambridge Health Alliance
- Consent form for study participation
Take our moral injury survey
The first part of our moral injury project consists of an intake survey to help us better understand the impact of financialization in U.S. health care, and how it intersects with racial health inequities. You can take our 10-minute survey at pnhp.org/survey.
Please note the following to better understand our survey process:
- Questions were developed in consultation with a working group of prominent physicians and academics, and through insights gleaned from a series of physician focus groups conducted over the summer of 2024.
- Our main audience for the survey is physicians who are currently practicing in the U.S., but we are collecting survey responses from all health professionals.
- We have secured Institutional Review Board (IRB) approval via Pearl IRB.
- This survey functions as an intake tool for a series of 1:1 interviews to be conducted over the spring/summer.
- We will release a high-level report of findings at PNHP’s 2025 Annual Meeting (Nov. 1-3 in Washington, D.C.), and will share this report with PNHP members, allies, and elected officials.
- We will author an academic paper detailing the results of our moral injury research, which will be submitted for journal publication at the end of 2025.
For reference, we have uploaded a PDF version of our complete moral injury survey HERE.
Share our moral injury survey
To properly understand the impact of financialization on U.S. health care, and how it intersects with racial health inequities, we will need to engage with thousands of currently practicing physicians. This means tapping our active PNHP members and going beyond this cadre of single-payer activists.
We need you to share the pnhp.org/survey link with currently practicing physicians in your network! To help you with this outreach, PNHP has put together a toolkit that includes:
- Moral injury project overview
- Sample email to recruit your colleagues
- Tips for sharing our survey in a professional setting
- Moral injury project flyer
- Frequently asked questions
We’ve also developed a one-page info sheet with information about our moral injury project.
Dr. Toby Terwilliger provides outreach tips
Respecting your privacy
PNHP’s moral injury survey covers delicate topics and gives participants the opportunity to share experiences from their practice—as well as experiences with specific employers, insurers, and other parties.
Rest assured that survey responses will be anonymized through the use of unique ID numbers and that nobody outside of PNHP’s survey team will ever have access to individual replies.
We also ask survey respondents to share their email address, so we can follow up regarding potential 1:1 interviews. Please note:
- Individuals who are not already in PNHP’s database can opt in to receive updates about our moral injury project.
- If respondents are added to our email list, they can unsubscribe at any time (link at the bottom of all PNHP emails).
- PNHP will never sell or share emails collected through our moral injury survey.
Moral injury workshop (Nov. 2024)
PNHP president Dr. Diljeet Singh helped lead a workshop on moral injury at our 2024 Annual Meeting in Chicago. Download Dr. Singh’s slideshow HERE.
The post Understanding Moral Injury in Health Care appeared first on PNHP.
2024 Annual Meeting Materials 4 Nov 2024 1:34 PM (5 months ago)
PNHP’s 2024 Annual Meeting in Chicago drew physicians, students, and health justice activists from across the country for a weekend of organizing, strategizing, and setting our agenda for the year ahead.
Please see below to access a selection of archival recordings, slideshows, and handouts from the meeting. To view photos from the meeting, visit our Flickr page.
During the conference, we encouraged attendees to post to social media using the hashtag #PNHP2024. Click HERE to read member tweets, and be sure to follow PNHP on Instagram, Twitter and Facebook for the latest on the Medicare for All movement.
Looking for materials from the Students for a National Health Program (SNaHP) Summit? Click HERE to access slideshows, photos, handouts, and more!
PNHP’s “Triple Aim” to advance our movement
PNHP president Phil Verhoef, MD, PhD kicked off our meeting by unveiling our “Triple Aim” of ending profiteering, improving traditional Medicare, and winning single payer (slideshow HERE).
Health Policy Update
PNHP past president Adam Gaffney, MD, MPH presented the latest data on the U.S. health crisis—from declining population health, to rampant profiteering, to onerous restrictions. Download Dr. Gaffney’s original slideshow HERE or an alternate visual presentation by Dr. Ed Weisbart HERE.
Bring Power to Truth: Fighting Medicare Advantage
SNaHP executive board members Shruthi Bhuma, M4 and Swathi Bhuma, M4 presented the main components of our campaign to stop Medicare profiteering: legislative, narrative, and organizing (slideshow HERE).
Welcome from Rep. Jan Schakowsky
Medicare for All cosponsor Rep. Jan Schakowsky (IL-9) welcomed PNHP members from across the country to Chicago, and urged us to keep pushing in the fight for single-payer reform.
Panel discussion: Reacting to the election
Featuring (R to L) Abdul El-Sayed, MD, DPhil; Alex Lawson, MPP; Wendell Potter; and A. Taylor Walker, MD, MPH. Moderated by Sanjeev Sriram, MD, MPH; and Emily Huff, M3
Workshops I: Campaigns for 2025
- Growing Power within Medical Societies, presented by Eve Shaprio, MD, MPH; Shannon Rotolo, PharmD; Stephen Kemble, MD; and Donald Bourne, M3 (worksheet HERE).
- Moral Injury: Let’s Talk About It, presented by Diljeet Singh, MD, DrPH; Carol Paris, MD; and Anand Habib, MD, MPhil (video recording HERE; slideshow HERE; worksheet HERE; moral injury survey HERE).
- A Toolbox for Building Local Power, presented by Toby Terwilliger, MD; Robel Worku; and Brooke Adams, M1 (worksheets HERE and HERE).
- Making Legislative Action Real, presented by Ed Weisbart, MD; Stephan Ramdohr; and Dan Doyle, MD (slideshow HERE; worksheet HERE).
Workshops II: Building Your Practical Skills
- Recruiting and 1:1: How to Utilize your Network, presented by Andy Hyatt, MD; Jessica Schorr Saxe, MD; and Alankrita Olson, MD (worksheet HERE).
- Tension is Part of Building Powerful Relationships of Accountability with our Legislators, presented by Hannah Willage; Belinda McIntosh, MD; and Lori Clark (slideshow HERE; worksheet HERE).
- Building Powerful Coalitions, presented by Betty Kolod, MD; Brian Yablon, MD; and Alex Newell-Taylor
- Communicating Clearly and Effectively, presented by Chiamaka Okonkwo, M4; Carol Paris, MD; Dixon Galvez-Searle; and Anika Thota (slideshow HERE; worksheet HERE; Dr. Paris’ letter to the editor HERE; moral injury survey HERE).
- Running Inclusive and Effective Meetings, presented by Zach Gallin, M4; Jenn Sugijanto, M4; and Morgan Moore (worksheets HERE and HERE).
Telling your personal health care story
Carol Paris, MD; Douglas Robinson, MD; Emily Thompson, MD; and Phil Lichtenstein, MD talk about their experiences in the exam room during our “Communicating Clearly and Effectively” workshop.
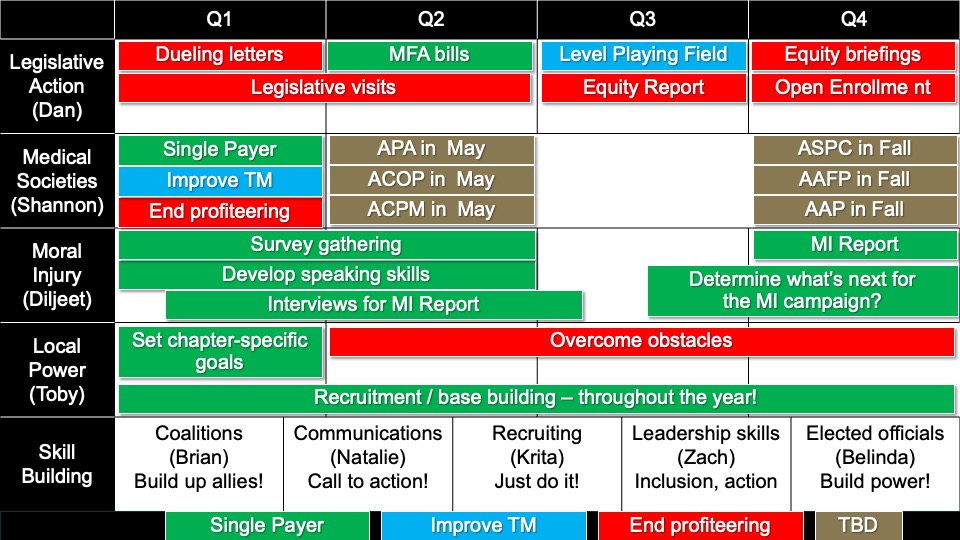
PNHP timeline for 2025
Developed by meeting attendees reporting back from our campaign and skill-building workshops. Built by Ashley Duhon, MD and Ed Weisbart, MD (recoding HERE; slideshow HERE).
Keynote: Rep. Pramila Jayapal
Congresswoman Pramila Jayapal, lead sponsor of the Medicare for All Act in the U.S. House and chair of the Congressional Progressive Caucus, concluded our meeting with a dinner keynote address.
Students for a National Health Program (SNaHP) Summit
Medical and health professional students convened in Chicago for the annual SNaHP Summit on Nov. 15, 2024. During registration, students took in a wide-ranging poster presentation in the lobby.
Organizing for Human Rights
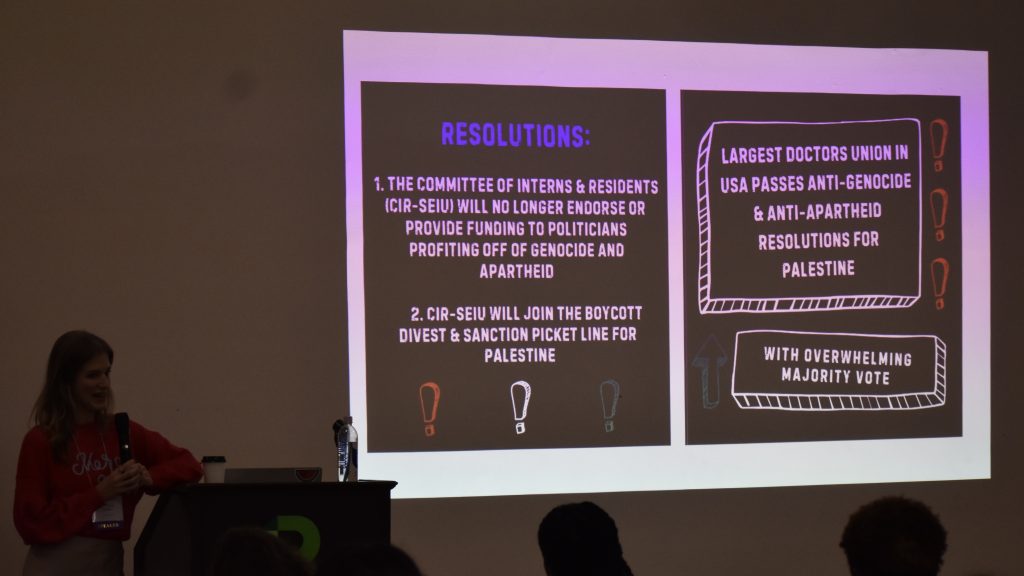
Committee of Interns and Residents president A. Taylor Walker, MD, MPH discussed her union’s organizing to pass two resolutions in support of Palestine.
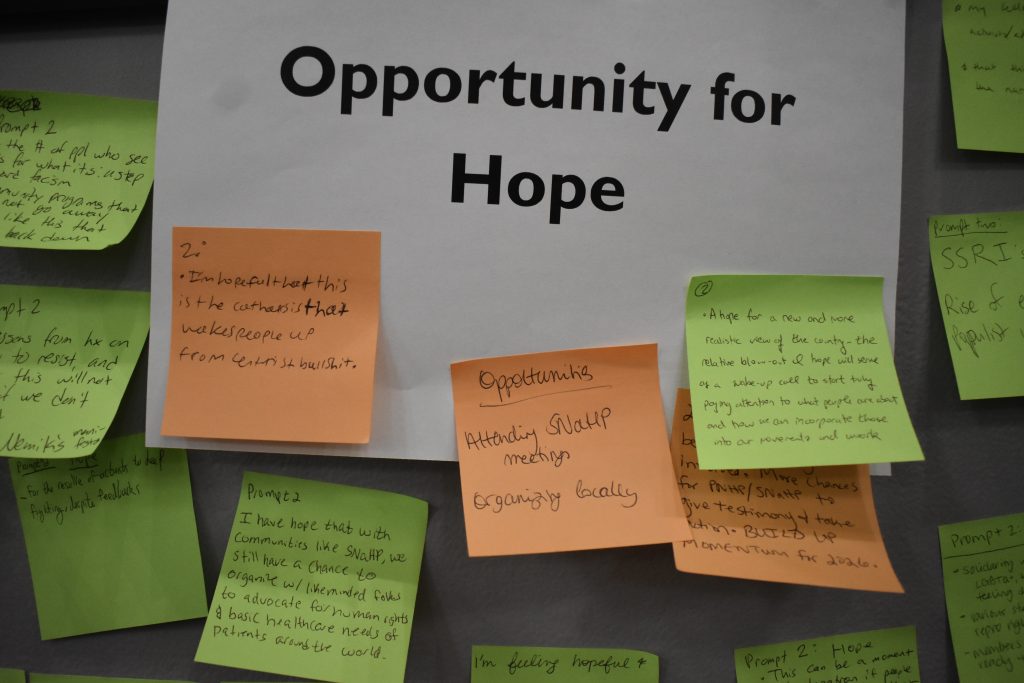
Debriefing the 2024 election
Patrick Haley and Chiamaka Okonkwo led an interactive session responding to the federal election. Students wrote down both their immediate reactions and what gave them hope in the moment.
Welcome from Rep. Delia Ramirez
Medicare for All cosponsor Rep. Delia Ramirez (IL-3) welcomed students from across the country to Chicago, the “birthplace of community organizing.”
Launching the NEW SNaHP website
SNaHP media team leaders Griffin Johnson and Natalie Koconis did their best Steve Jobs impressions while launching the revamped student.pnhp.org website.
SNaHP Strategy in 2025
The SNaHP Summit started in earnest with presentations by Michael Massey (introduction, slideshow HERE); Shruthi and Swathi Bhuma (welcome to Chicago, slideshow HERE); Cortez Johnson (roll call); Max Brockwell and James Waters (strategic vision, slideshow HERE); and PNHP president Phil Verhoef, MD, PhD (Triple Aim, slideshow HERE).
Breakout Sessions I
- Building Statewide/Regional SNaHP Power, presented by Samuel Marquina, Gitanjali Lakshminarayanan, Carson Hartlage, Laureen Haack, and Helen Bassett (slideshow HERE)
- Start with Empathy: Talking Progress with Conservatives, presented by Cortez Johnson and John Kearney (slideshow HERE)
- Becoming Us: Building Power through Effective 1:1, presented by Andrew Meci and Annabelle Brinkerhoff (slideshow HERE; worksheet HERE)
- Writing Letters to Legislators, presented by Nina Silver, Halima Suleiman, and Priya Patel (slideshow HERE)
- The Labor Movement in Medicine: Lessons for Organizers, presented by Kevin Hu, Tom Statchen, Andy Hyatt, and A. Taylor Walker (slideshow HERE)
Breakout Sessions II
- Building A Powerful SNaHP Chapter, presented by Patrick Haley, Pritom Karmaker, and Mariam Tadross (slideshow HERE)
- The Power of Campaign Building and Plans: How We Win, presented by Max Brockwell and Chiamaka Okonkwo (slideshow HERE)
- Building knowledge about single-payer inside and outside of your med school curriculum, presented by Michael Massey and Constance Fontanet (slideshow HERE; worksheet HERE)
- Post Election Debrief: Connect, Reflect, What’s Next, presented by James Moore and Wade Catt (slideshow HERE)
- Becoming Us: Developing Powerful Testimony, presented by Donald Bourne, Carson Hartlage, Emily Huff, Allison Benjamin, Ksenia Varlyguina, and Mo Kinsinger (slideshow HERE)
Call to Action!
Shruthi and Swathi Bhuma (slideshow HERE); Allison M. Benjamin and Nina Silver; and Michael Massey led an interactive session where students made commitments to build power, take action, and work towards our North Star of Medicare for All.
The post 2024 Annual Meeting Materials appeared first on PNHP.
PNHP National Office Staff 23 Aug 2024 10:07 AM (7 months ago)
 Ken Snyder – Executive Director
Ken Snyder – Executive Director
Contact for: organizational strategy; legislative and external relations; Board of Directors; development. Phone extension: 6025
 Matthew Petty – Deputy Director
Matthew Petty – Deputy Director
Contact for: memberships and donations; PNHP Annual Meeting; organizational operations and finance; human resources. Phone extension: 6024
 Lori Clark – National Organizer
Lori Clark – National Organizer
Contact for: membership committee; pediatricians Member Interest Group (MIG); chapters in CA, FL, GA, ME, MD, MA, OH; Students for a National Health Program (SNaHP). Phone extension: 6021
 Rebecca Delay – National Organizer
Rebecca Delay – National Organizer
Contact for: specialty-based Member Interest Groups (MIGs); medical society resolutions; medical conferences; Grand Rounds; chapters in AZ, CO, IL, IN, KY, MI, MN, NM, OR, PA, TN, TX, VA. Phone extension: 6020
 Mandy Strenz – National Organizer
Mandy Strenz – National Organizer
Contact for: anti-profiteering and Medicare (dis)Advantage campaign; membership committee; events calendar; chapters in AK, CT, DC, HI, IA, LA, MO, NH, NJ, NY, NC, ND, PR, RI, SC, VT, WA, WV, WI. Phone extension: 6026
 Dixon Galvez-Searle – Communications Specialist
Dixon Galvez-Searle – Communications Specialist
Contact for: email communications; social media (Facebook, Instagram, LinkedIn, and X/Twitter); website updates; branding and design. Phone extension: 6022
 Anika Thota – Policy and Communications Specialist
Anika Thota – Policy and Communications Specialist
Contact for: press inquiries; print and broadcast media; policy committee; policy questions. Phone extension: 6023
For a list of PNHP officers, directors, advisers, and past presidents, please see our Board of Directors page.
The post PNHP National Office Staff appeared first on PNHP.
2024 Annual Meeting 25 Jun 2024 11:49 AM (9 months ago)
Register HERE for the Nov. 16 meeting!
Note: Online registration will close on Sunday, Nov. 10 at 11:59 pm Central. Because of high demand, registration at the door may be limited.
PNHP Annual Meeting
Saturday, Nov. 16 (agenda available HERE)
- Daytime program, 9:00 am – 5:00 pm
- Dinner program, 6:00 pm – 8:00 pm
The PNHP Annual Meeting will be held in Chicago at the Venue SIX10, located at 610 S. Michigan Ave.
Sleeping rooms will be available at the Hilton Chicago, 720 S. Michigan Ave., for $229/night + $25/night mandatory destination charge (includes internet and athletic club access, and $25/day food/beverage credit). Sleeping room reservations may be booked in two ways:
- Online HERE
- Call 877-865-5320 and reference “PNHP Annual Meeting”
Sleeping room reservations must be made by Friday, Oct. 25. Note that the Hilton is completely booked for nights after Nov. 17.
SNaHP Summit
Friday, Nov. 15, 12:00 pm – 6:00 pm
The SNaHP Summit will be held in Chicago at Roosevelt University, located at 430 S. Michigan Ave. This event is not affiliated with Roosevelt University.
Scholarships are available to support student and resident attendance for both the SNaHP Summit and the PNHP Annual Meeting. Please note that the application deadline has passed, and we are in the process of awarding scholarships to qualified applicants. PNHP members and the public can support PNHP’s student outreach programs by making a GIFT to the Nicholas Skala Student Fund.
Speakers
 Dinner Keynote: Rep. Pramila Jayapal
Dinner Keynote: Rep. Pramila Jayapal
Congresswoman Pramila Jayapal represents Washington’s 7th District in the U.S. House and is chair of the Congressional Progressive Caucus and co-lead sponsor of the Medicare for All Act.

Meeting Chair: Dr. Philip Verhoef
Dr. Phil Verhoef is the president of PNHP, an adult and pediatric intensivist, and a clinical associate professor of medicine at the John A. Burns School of Medicine at the University of Hawaii-Manoa.
Health Policy Update:
- Dr. Adam Gaffney, Past President, PNHP; Assistant Professor of Medicine, Harvard Medical School
- Shruthi Bhuma, executive board member, SNaHP; board advisor, PNHP; M4, Chicago Medical School
- Swathi Bhuma, executive board member, SNaHP; board member, PNHP; M4, Chicago Medical School
Plenary Discussion Panel:
- Dr. Abdul El-Sayed, County Public Health Director, host of the America Dissected podcast, and author of Healing Politics and Medicare for All
- Alex Lawson, Executive Director, Social Security Works
- Wendell Potter, President, Center for Health and Democracy
- Dr. A. Taylor Walker, President, Committee of Interns and Residents
See our agenda for a full lineup of speakers and workshops.
This conference will not be livestreamed in its entirety, but recordings of select sessions will be made available after the meeting.
Covid Safety Protocols
Please note that our medical experts recommend the following Covid safety precautions for the conference:
- Staying home if you are experiencing symptoms suggestive of Covid, such as a sore throat, persistent cough, or fever
- Testing immediately before the conference
- Vaccination, particularly with one of the updated vaccines covering newer strains
- Wearing a face mask while not actively eating or drinking
Previous Annual Meetings
Click HERE to access archival material from last year’s Annual Meeting in Atlanta. Click HERE to view photos from the conference.
Attending the 2024 PNHP Annual Meeting and SNaHP Summit is entirely voluntary and requires attendees to abide by any applicable rules of conduct, or local or state laws, that may be announced at any time. Attendees acknowledge the highly contagious and evolving nature of Covid-19 and voluntarily assume the risk of exposure to, or infection with, the virus by attending the Meeting, and understand that such exposure or infection may result in personal injury, illness, disability, and/or death. Attendees release and agree not to sue any persons or entities responsible for coordinating or organizing the PNHP Annual Meeting and SNaHP Summit in the event that they contract Covid-19. Attendees agree to comply with all Covid-related procedures that may be implemented at the Meeting, including mask-wearing.
The post 2024 Annual Meeting appeared first on PNHP.
PNHP Newsletter: Spring 2024 24 Jun 2024 2:18 PM (9 months ago)
Table of contents
Click the links below to jump to different sections of the newsletter. To view a PDF version of the shorter print edition of the newsletter, click HERE.
If you wish to support PNHP’s outreach and education efforts with a financial contribution, click HERE.
If you have feedback about the newsletter, email info@pnhp.org.
PNHP News and Tools for Advocates
- PNHP Leads Fight Against Medicare Advantage
- PNHP Caps off 35th Anniversary at Annual Meeting
- Heal Medicare: PNHP Launches Revamped Website
- Meet Mandy, Our New National Organizer
Save the Date for our Annual Meeting in Chicago
Research Roundup
- Data Update: Health care crisis by the numbers
- Studies and analysis of interest to single-payer advocates
PNHP Chapter Reports
SNaHP Chapter Reports
Reclaiming Medicare for the Public
PNHP in the News
PNHP News and Tools for Advocates
PNHP Leads Fight Against Medicare Advantage
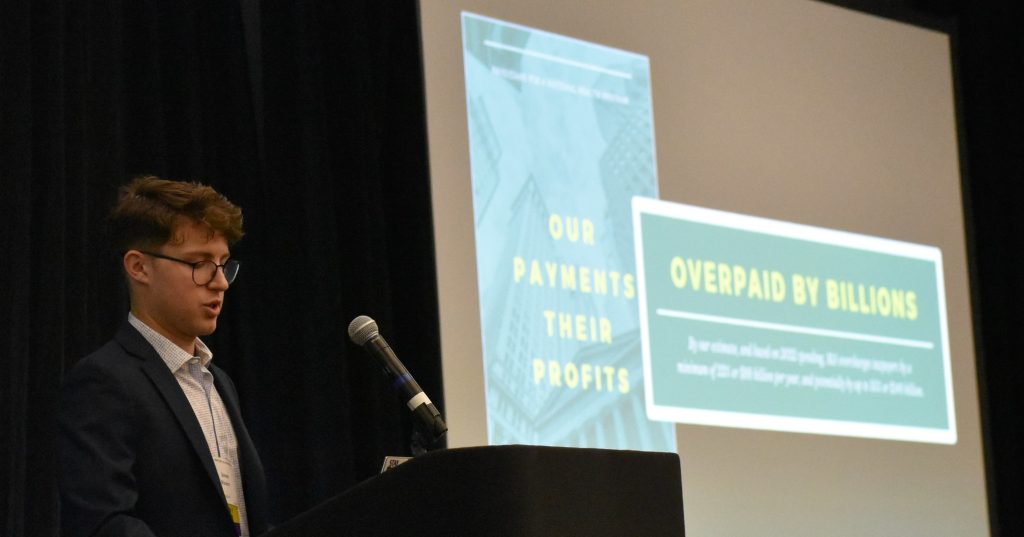
As controversies continue to build around the corporate-run Medicare Advantage (MA) program, PNHP has become a leader in the fight to crack down against its abuses and strengthen Traditional Medicare. First, in October, PNHP released a report quantifying the egregious levels of overpayments in the program. This report was covered extensively in the media and used in briefings with members of Congress, and has set the standard for discussing MA’s raiding of the Medicare Trust Fund.
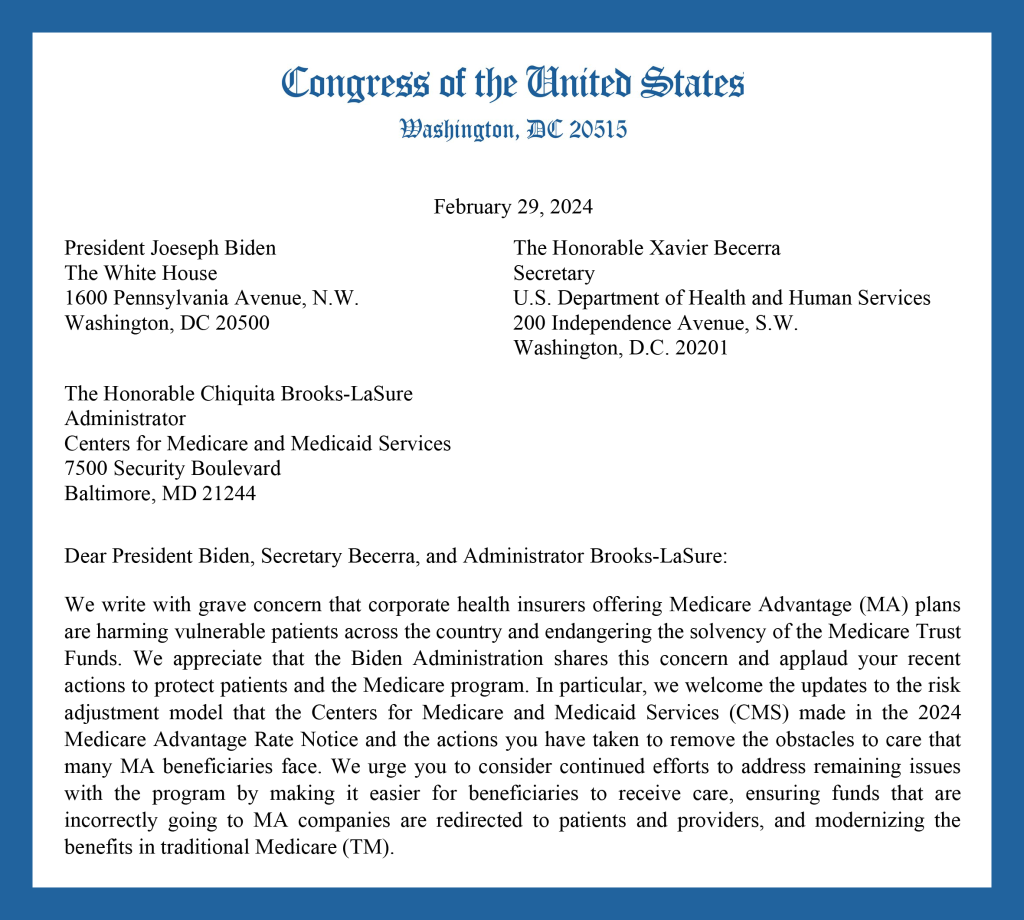
Beginning in January, PNHP chapters around the country began organizing efforts around two different letters circulating in both chambers of Congress regarding Medicare Advantage. One letter was sponsored by the insurance industry, and uncritically praised MA while calling for increased support for the program. The other letter, written by progressive members of Congress like Rep. Pramila Jayapal, Rep. Rosa DeLauro, Rep. Jan Schakowsky, Sen. Elizabeth Warren, and Sen. Sherrod Brown, outlined the many flaws in MA and the critical need to reform the program while improving benefits in Traditional Medicare.
PNHP staff, members, and allied organizations set up dozens of meetings with their Congressional representatives to ask them not to sign on to the pro-industry letter, and to instead sign on to the reform letter. PNHP members helped lead over 40 meetings with members of both the House and Senate, and were able to convince several members to sign on to the reform letter that had not done so the previous year. In total, around 50 House members and 10 Senate members signed onto the reform letter.
Alongside our organizing campaign, PNHP also conducted an extremely successful email campaign urging members to contact their representatives with a message about the two MA letters. Almost 20,000 messages were sent through our email form, sending a strong signal to members of Congress that their constituents care deeply about the need to protect Medicare from privatization.
PNHP’s campaign against Medicare Advantage will continue through the year. If you would like to get involved, please contact National Organizer Mandy Strenz at mandy@pnhp.org.
PNHP Caps off 35th Anniversary at Annual Meeting

After a year of celebrating PNHP’s 35th Anniversary through organizing, fundraising, and activism, we capped everything off at our Annual Meeting in Atlanta. Things kicked off on Friday with the Leadership Training, featuring presentations and workshops from leaders in PNHP and SNaHP. On Saturday morning, the Annual Meeting opened with the always hotly anticipated Health Policy Update, delivered by PNHP past president Dr. Adam Gaffney and SNaHP executive board member James Patrick Waters. They touched on a wide range of topics, including declining life expectancy, the ongoing Medicaid unwinding, and the dangerous expansion of Medicare Advantage.
After another day of workshops on topics ranging from organizing to moral injury to reproductive justice, attendees gathered for this year’s keynote address, delivered by distinguished physician activist and former American Public Health Association president Dr. Camara Jones. Dr. Jones gave a thought-provoking and allegory-rich talk on recognizing and combating racial inequity, both in health and in U.S. society more broadly.
Saturday night’s highlight was the 35th Anniversary Dinner. Members took the stage to reminisce on three-and-a-half decades of fighting for health care justice with PNHP, and to recognize national allies, past presidents, medical student leaders, and co-founders. At the end of the dinner, the Quentin Young and Nick Skala health activist awards were presented to Dr. George Bohmfalk, Dr. Diljeet Singh, and SNaHP leader Donald Bourne.
Sunday saw our SNaHP members gathered for their annual Student Summit—running their own workshops and learning from one another about activism and leadership. To end the weekend, meeting attendees piled into buses and headed off to a fantastically organized public action protesting hospital closures and demanding Medicaid expansion in Georgia. The action was even covered by the Atlanta Journal-Constitution!
PNHP’s 35th anniversary initiatives were to build the future of our movement by supporting the work of SNaHP; ramping up our fight against corporate profiteering, with a particular focus on the so-called “Medicare Advantage” program; and greatly increasing our base of active physician members fighting for improved Medicare for All. We made substantial progress in all these areas in 2023, and will continue to do so in 2024.
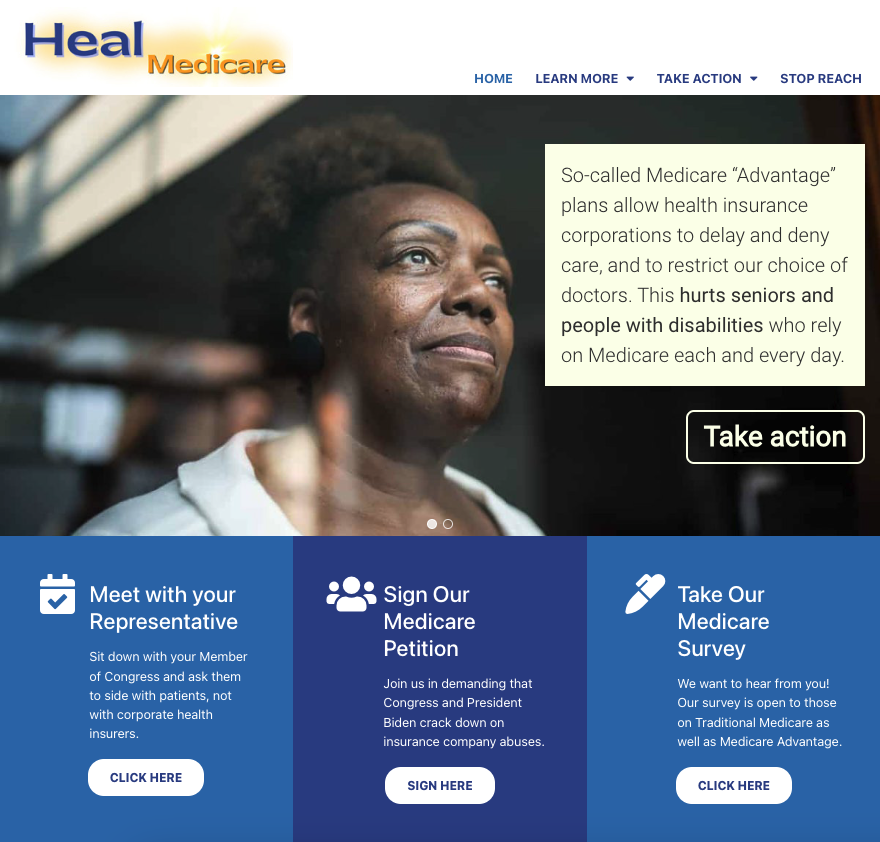
Heal Medicare: PNHP Launches Revamped Website
As part of PNHP’s campaign against Medicare profiteering, we have created a new website to help activists wade through the many complex issues related to both traditional Medicare and corporate-controlled Medicare Advantage (MA) plans. The new website is called HealMedicare.org, and contains many resources to help explain the dangers of MA, and how we can collectively fight back.
The two focuses of the website are education (clearly explaining the harm caused by corporations like Cigna, Aetna, and UnitedHealthcare) and activism (raising our voices and organizing an effective response). The website has already been used extensively in our 2024 MA letter campaign, and contains a legislative toolkit with a robust set of links, documents, and videos for anyone looking to engage their representatives.
We will continue to update the site as our campaign evolves throughout the year. Please take a look, and share with anyone who is concerned for the future of our public Medicare!
Meet Mandy, Our New National Organizer

Previous Experience: I worked with PNHP-NY Metro as the Chapter Coordinator starting in 2021 – and before that in the fine jewelry world, with advocacy work solely in my spare time.
What drew you to PNHP? Healthcare access is a throughline in many issues I care about: climate, immigration, reproductive rights, anti-war efforts, LGBTQIA+ issues, etc. While single payer alone wouldn’t solve any of those issues, it has the potential to majorly alleviate some of the strain people feel around them. Also, I just love getting to work on things I care about every day, especially with people as committed as PNHP members are.
What are you looking forward to working on over the next 12 months? I’m looking forward to seeing PNHP chapters grow their power and influence both locally and nationally.
What’s a fun fact about yourself? I’ve yet to meet a fermented food I don’t adore – please give me some challenging ones to try!
Thanks to the generosity of donors to our 35th anniversary campaign, Mandy Strenz joins PNHP as the third member of our growing Organizing Team alongside Lori Clark and Rebecca Delay. Connect with Mandy at mandy@pnhp.org.
Save the Date for our Annual Meeting in Chicago
Join us for PNHP’s Annual Meeting, scheduled for Saturday, Nov. 16 in Chicago at the Venue SIX10, located at 610 S. Michigan Ave.
Our annual Students for a National Health Program (SNaHP) Summit is scheduled for the preceding day (Friday, Nov. 15) at a TBD location in Chicago. Stay tuned for more information, including registration, at pnhp.org/meeting.

Research Roundup
Data Update: Health Care Crisis by the Numbers
Barriers to Care
Ketamine can be lifesaving, but is difficult to access: Although increasingly popular as an option for treatment-resistant depression, IV Ketamine treatments for mental illness are currently off-label and thus rarely covered by insurers, costing anywhere from $400 to $1000 per treatment. Esketamine, a nasal spray and the only ketamine drug approved for depression, carries an out-of-pocket cost of $784 a month for two inhalers. Emily Maloney, “Ketamine can be transformative for people with suicidal thoughts — if they can access it,” STAT News, 9/7/23.
Insurers deny critical treatment for eating disorders: In deciding whether to cover eating disorder treatment, insurers often emphasize metrics like weight and body mass index while minimizing patients’ serious psychiatric symptoms. For example, a teen couldn’t get her insurer to cover her eating disorder and suicidality, even after three separate clinicians vouched for her admission to a specialty program. In terms of total costs, a hospital stay for eating disorder treatment runs an average of $61,000. Of the 20 most expensive psychiatric stays among Washington youth in 2021, 40% involved those with an eating disorder. Hannah Furfaro, “Not sick enough: How insurance denials can delay lifesaving eating-disorder treatment,” Seattle Times, 9/10/23.
Abortion coverage limited or unavailable at many employers: Around one-fourth of large U.S. employers heavily restrict coverage of legal abortions or don’t cover them at all under health plans for their workers. 10% of large employers don’t cover abortion at all, and 18% cover it only in limited circumstances. In 2021, the median costs for people paying out-of-pocket in the first trimester were $568 for a medication abortion and $625 for an abortion procedure. By the second trimester, the cost increased to $775 for abortion procedures. Rachana Pradhan, “Abortion Coverage Is Limited or Unavailable at a Quarter of Large Workplaces,” KFF Health News, 10/18/23.
Insurance premiums rise for U.S. families: Premiums rose 7%, compared to just a 1% increase last year. The average premium is now just under $24,000 for families who get their coverage through employers (about 153 million people in the United States are covered under this type of insurance) The 7% increase is the largest since 2011, and was at least partially driven by high inflation. Cailley LaPara, “Health Insurance Premiums Now Cost $24,000 a Year, Survey Says,” Bloomberg, 10/18/23.
Large numbers of Americans struggle to pay for care: 43% of those with employer coverage, 57% with marketplace or individual-market plans, 45% with Medicaid, and 51% percent with Medicare said it was very or somewhat difficult to afford their health care. 54% percent of people with employer coverage who reported delaying or forgoing care because of costs said a health problem of theirs or a family member got worse because of it, as did 61% in marketplace or individual-market plans, 60% with Medicaid, and 63% with Medicare. Sara R. Collins et al., “Paying for It: How Health Care Costs and Medical Debt Are Making Americans Sicker and Poorer,” Commonwealth Fund, 10/26/23.
Child survivors of shootings face huge costs: Survivors’ health care spending increased by an average of $34,884—a 17.1-fold increase. Parents of survivors experienced a 30–31% increase in psychiatric disorders, with 75% more mental health visits by mothers, and 5–14% reductions in mothers’ and siblings’ routine medical care. Family members experienced substantially larger 2.3- to 5.3-fold increases in psychiatric disorders, with at least 15.3-fold more mental health visits among parents. Zirui Song et al., “Firearm Injuries In Children And Adolescents: Health And Economic Consequences Among Survivors And Family Members,” Health Affairs, November 2023.
Long term care causes dire financial issues: Among Americans who had $171,365 to $1.8 million in savings at age 65, those with greater long-term care needs were much more likely to deplete their savings than those who did not need long-term care. 23.6% of those who lived in a nursing home died broke. The median annual cost of a private room in a nursing home was over $100,000 in 2020, and a home health aide costs over $60,000. Six in 10 adults age 50 and older feel “mostly” or “somewhat anxious” about affording the cost of a nursing home, assisted living facility, paid nurse, or aide to assist them in retirement. Reed Abelson and Jordan Rau, “Facing Financial Ruin as Costs Soar for Elder Care,” KFF Health News, 11/14/23.
Thousands of U.S. rape victims unable to get an abortion: 65,000 rape-related pregnancies occurred in the 14 states which have passed near-total abortion bans since the Dobbs decision in 2022. Even for those states which provide exceptions for rape, abortions are extremely difficult to access. Texas alone, owing to its large population and total banning of abortion without exceptions, accounted for approximately 26,000 of these pregnancies. Jessica Glenza, “Nearly 65,000 US rape victims could not get an abortion in their state, analysis shows,” The Guardian, 1/25/24.
GoFundMe remains critical to paying for care: The annual number of U.S. campaigns on GoFundMe related to medical causes (about 200,000) was 25 times the number of such campaigns on the site in 2011. The company has estimated that roughly a third of the funds raised on the site are related to costs for illness or injury, but that could be an undercount as some campaigns are counted under different categories. Campaigns made an average of about 40% of the target amount, and there is evidence that this number has worsened over time. Elisabeth Rosenthal, “GoFundMe Has Become a Health Care Utility,” KFF Health News, 2/12/24.
Medicare & Medicaid Issues
Unenrolled Medicaid-eligible adults have difficulty accessing care: 37% of adults who are eligible for Medicaid but not enrolled in the program and do not have private insurance report having a usual source of care, compared to 69.9% of Medicaid enrollees and 66.8% of Medicaid-eligible individuals with private insurance. Unenrolled Medicaid-eligible individuals are more likely to delay care due to cost concerns (21.4% compared to 7.3% of Medicaid enrollees and 9.5% of Medicaid-eligible individuals with private insurance). Compared to Medicaid enrollees, unenrolled eligible adults were also less likely to have visited a doctor within the last year (23.4% vs 65.4%), had a prescription filled (27.8% vs 67%), or stayed in a hospital (2.5% vs 12.6%). Bowen Garrett et al., “Medicaid-Eligible Adults Who Lack Private Coverage and Are Not Enrolled,” Urban Institute, August 2023.
Beneficiaries in Medicare Advantage report affordability problems: 22% of Medicare Advantage (MA) enrollees reported high health care costs that made them underinsured, compared with 13% on Traditional Medicare plus supplemental coverage. 21% of MA enrollees reported problems paying medical bills and debt, compared with 14% of those on Traditional Medicare. Despite the touting of dental benefits as part of MA plans, 30% of those with MA reported delaying or not getting dental care due to cost. Faith Leonard et al., “Medicare’s Affordability Problem: A Look at the Cost Burdens Faced by Older Enrollees,” Commonwealth Fund, 9/19/23.
Georgia Medicaid enrollment is low: The program, which is known as Pathways and has work requirements, has only enrolled 1,343 residents in the 3 months since it began. The state previously said it delayed the reevaluations of 160,000 people who were no longer eligible for traditional Medicaid but could qualify for Pathways to help them try to maintain health coverage. But observers have said they have detected little public outreach to target populations. In addition to imposing a work requirement, Pathways limits coverage to able-bodied adults earning up to 100% of the poverty line, which is $14,580 for a single person or $30,000 for a family of four. Associated Press, “Georgia Medicaid program with work requirement has enrolled only 1,343 residents in 3 months,” 10/20/23.
Rural hospitals feel sting of Medicare Advantage growth: MA enrollment has increased fourfold in rural areas since 2010. However, its growth has imperiled the finances of small hospitals in these more remote regions, as their payments are often lower than traditional Medicare and are regularly delayed or never arrive from insurers. One profiled hospital, Mesa View, is owed $800,000 by MA plans for care already provided. Sarah Jane Tribble, “Tiny, Rural Hospitals Feel the Pinch as Medicare Advantage Plans Grow,” KFF Health News, 10/23/23.
Halfway through Medicaid unwinding, millions disenrolled: Of the 94 million people enrolled in Medicaid and CHIP in March 2023, at the end of January, 32 million have renewed coverage and 16 million have been disenrolled. Since the start of unwinding, Medicaid enrollment has declined in every state, ranging from 32% in Idaho to 1% in Maine. Bradley Corallo, “Halfway Through the Medicaid Unwinding: What Do the Data Show?” KFF, 1/30/24.
Medicare Advantage profitability is down: Between 2019 and 2022, the profit margin in MA declined from 4.9% to 3.4%, while earnings per member declined 28%. Increased utilization is partially responsible; UnitedHealth posted its largest medical loss ratio of 85% in the fourth quarter of 2023. Humana, which relies heavily on Medicare Advantage for its business model, reported profits falling far short of expectations in its latest release and has lowered its guidance for the coming year to $16 in adjusted earnings per share. Its stock fell over 14% after the release of its last earnings report. Emily Olsen, “Medicare Advantage profitability is declining, Moody’s says,” Healthcare Dive, 1/30/24.
MA enrollees report issues with care and benefits: Larger shares of beneficiaries in MA plans than in traditional Medicare reported they experienced delays in getting care because of the need to obtain prior approval (22% vs. 13%) and couldn’t afford care because of copayments or deductibles (12% vs. 7%). 31% of MA beneficiaries reported using none of their supplemental benefits in the past year. Gretchen Jacobson et al., “What Do Medicare Beneficiaries Value About Their Coverage?” Commonwealth Fund, February 22, 2024.
MA home health patients get less care: The study compared more than 285,000 patients receiving home health care through MA and TM from 102 home health locations in 19 states. MA patients had a shorter home health length of stay by 1.62 days, and received fewer visits from all disciplines except social work. There were no differences between the two types of Medicare in inpatient transfers. MA patients had 3% and 4% lower adjusted odds of improving in mobility and self-care, respectively. MA patients were 5% more likely to discharge to the community compared with TM. Rachel A. Prusynski et al., “Differences in Home Health Services and Outcomes Between Traditional Medicare and Medicare Advantage,” JAMA Health Forum, March 1, 2024.
Pharma
States taking steps to reduce drug prices: As Medicare prepares to begin negotiating drug prices, states are taking matters into their own hands using Prescription Drug Affordability Boards. These boards set upper limits for prices paid by state and local governments, and sometimes even for commercial health plans as well. For instance, the Minnesota board will review select brand-name drugs or biologics for which the list price rose by more than 15% or more than $2,000 during any 12-month period or course of treatment lasting under 12 months. Ed Silverman, “Medicare may plan to negotiate drug prices, but some states are taking their own steps to lower costs,” STAT News, 10/11/23.
Insurers begin charging for COVID treatment: Paxlovid, the most popular antiviral COVID treatment, was covered by the government free of charge until the end of 2023. Pfizer announced that it would set the price for the drug at $1390 per course. When the U.S. government was purchasing the drug, it paid around $530 per course. The United States purchased around 24 million courses of Paxlovid. About 3.4 million doses had been given in 2023 at the time of the announcement. Michael Erman, “Pfizer to price COVID treatment Paxlovid at $1,390 per course,” Reuters, 10/18/23.
Sickle cell therapies are costly: The newly approved drugs, the first CRISPR-based gene therapies approved by the FDA, are known as Casgevy and Lyfgenia. Casgevy is priced at $2.2 million, while Lyfgenia has an even higher price of $3.1 million. These one-time therapies have prices comparable to the lifetime estimated cost of managing sickle cell disease, estimated at between $4 and $6 million. Many of the approximately 16,000 people estimated to be eligible for Casgevy in the U.S. are covered by Medicaid, which may be limited in its ability to cover the drug. Ned Pagliarulo, “Pricey new gene therapiest for sickle cell pose access test,” Biopharma Dive, December 8, 2023.
Pharma companies use patents to stifle competition: A study in JAMA found that pharmaceutical companies use “terminal disclaimers” to create “patent thickets” by filing dozens of patents on drugs that protect little of true value, but allow companies to sue to prevent the production of generic or biosimilar drugs. 48% of the 271 drug patents currently in litigation involved the use of terminal disclaimers. An analysis found a 200% increase in patents filed by companies that made few substantive changes to their drugs. From 2000 to 2015, the FDA approved 1,421 new drugs. The ratio of continuation patents increased from 0.6 in 2000 to 1.8 in 2015. These practices allow pharmaceutical companies to keep exclusivity for their drugs and keep their prices high. Ed Silverman, “Patent thickets and terminal disclaimers: How pharma blocks biosimilars from the marketplace,” STAT News, December 21, 2023.
Insulin becomes cheaper for many Americans: The three major insulin manufacturers have lowered the cost of insulin to $35 a month for most patients, and Medicare enrollees pay no more than $35 a month as part of provisions of the Inflation Reduction Act. The inflation-adjusted cost of insulin has increased 24% between 2017 and 2022. An estimated 8.4 million Americans rely on insulin to survive, and as many as 1 in 4 patients have been unable to afford their medicine. Experts have noted that manufacturers’ lowering of prices coincides with changes to Medicaid rebate rules that mean these companies will save hundreds of millions by lowering the price of their drugs. One of the companies, Eli Lilly, could avoid having to pay an additional $430 million in Medicaid rebates in 2024 by lowering their insulin price. Tami Luhby, “More Americans can now get insulin for $35,” CNN, January 2, 2024.
Senate Democrats investigate asthma inhaler prices: In the past five years, AstraZeneca, GlaxoSmithKline (GSK), and Teva made more than $25 billion in revenue from inhalers alone. One of AstraZeneca’s inhalers costs $645 in the U.S. but just $49 in the U.K. One of Boehringer Ingelheim’s inhalers costs $489 in the U.S. but just $7 in France. GSK’s Advair HFA costs $319 in the U.S. but just $26 in the U.K. About 25 million Americans have asthma, and about 16 million have chronic obstructive pulmonary disease (COPD), two conditions that could require the use of inhalers. Nathaniel Weixel, “Sanders, Democrats launch investigation into asthma inhaler pricing,” The Hill, 1/8/24.
Drugmakers hike prices on over 700 medications: The average price increase across the industry was about 4.5% at the beginning of 2024, slightly behind previous averages of about 5%. Two notable increases include Ozempic and Mounjaro, the weight-loss drugs that have exploded in popularity. Ozempic’s price rose 3.5% to $984.29 for a month’s supply, while Mounjaro rose 4.5% to about $1,000 for a month’s supply. Other increases listed include pain medication Oxycontin (9%), blood thinner Plavix (4.7%), and antidepressant Wellbutrin (9.9%). Aimee Picchi, “Drugmakers hiking prices for more than 700 medications, including Ozempic and Mounjaro,” CBS News, 1/18/24.
Americans pay more for drugs than people in other countries: Across all drugs, U.S. prices were 278% of comparison countries’ prices. U.S. gross prices for brand-name originator drugs were 422% of comparison country prices. The only category where Americans spent less was in unbranded generics, which accounted for 90% of U.S. prescription drug volume but only 8% of spending (compared to 41% of volume and 13% of spending for comparison countries). By contrast, brand-name originator drugs accounted for only 7% of U.S. prescription drug volume, but 87% of U.S. prescription drug spending (compared with 29% of volume and 74% of spending in comparison countries). Andrew W. Mulcahy, “International Prescription Drug Price Comparisons,” RAND Corporation, February 1, 2024.
Health Inequities
Racial disparities in access to care for chronic pain among opioid addicts: A study of Medicare beneficiaries with chronic lower back pain and opioid use disorder found disparities in the time to receive chiropractic care. Median time to chiropractic care was longest for American Indian or Alaska Native people at 8.5 days, followed by Black or African American people at 7 days, and shortest for Asian or Pacific Islander people at 0 days. After adjustment, Black or African American and Hispanic people had lower odds of receiving chiropractic care within 3 months of diagnosis compared with non-Hispanic White persons. Fiona Bhondoekhan et al., “Racial and Ethnic Differences in Receipt of Nonpharmacologic Care for Chronic Low Back Pain Among Medicare Beneficiaries With OUD,” JAMA Network Open, 9/12/23.
Unionized nursing homes more likely to report worker issues: From 2016-2021, the compliance rate for reporting workplace injuries and illnesses in nursing homes was only 40%. A study found that two years after unionization, nursing homes were 31.1% more likely than nonunion nursing homes to report workplace injury and illness data to OSHA. Further unionization could help improve workplace safety in nursing homes, a sector with one of the highest occupational injury and illness rates in the US. Adam Dean et al., “The Effect Of Labor Unions On Nursing Home Compliance With OSHA’s Workplace Injury And Illness Reporting Requirement”, Health Affairs, September 2023.
Pharmacy deserts grow in vulnerable communities: Rite Aid, CVS, and Walgreens have announced plans to collectively close an estimated 1500 stores. These store closures often hit low-income Black and Latinx neighborhoods first. An estimated 1 in 4 neighborhoods are pharmacy deserts across the country. Although the number of pharmacies in the United States has stayed at around 64,000 since 2014, pharmacies are increasingly leaving low-income and majority Black and Latinx neighborhoods and expanding in predominantly White and middle to higher-income areas, widening gaps in access. Aaron Gregg and Jaclyn Peiser, “Drugstore closures are leaving millions without easy access to a pharmacy,” Washington Post, October 22, 2023.
Young black males with ADHD are underdiagnosed and undertreated: The odds that Black students got diagnosed with the neurological condition were 40% lower than for white students, with all else being equal. For young black males, the odds were 60% lower. Black children are 2.4 times as likely as white kids to receive a diagnosis of conduct disorder compared with a diagnosis of ADHD. Claire Sibonney, “Underdiagnosed and Undertreated, Young Black Males With ADHD Get Left Behind,” KFF Health News, 11/9/23.
Disparities in infant mortality rate persist in Alabama: Although Alabama’s overall infant mortality rate fell from 7.6 deaths per 1000 live births in 2021 to 6.7 deaths in 2022, the gap between Black and white infant mortality persisted. Among Black mothers, the rate actually increased from 12.1 in 2021 to 12.4 in 2022, while for white mothers it dropped from 5.8 in 2021 to 4.3 in 2022. Summer Harrell, “Alabama sees decrease in infant mortality rate, but racial disparities persist,” ABC 33/40, 11/16/23.
Black Medicaid heart failure patients more likely to be hospitalized: 12.7 percent of Black patients who were previously diagnosed with heart failure and could enroll in Medicaid through the Supplemental Security Income (SSI) program had a preventable hospitalization. This is nearly twice the rate of white enrollees with heart failure, of which about 7.2 percent experienced preventable hospitalizations. This effect was present in the pooled sample of 11 states for which race of patients could be assessed. In general for heart failure, asthma/COPD, and diabetes, preventable hospitalization rates were substantially higher for adults eligible for Medicaid through SSI compared with adults eligible for Medicaid through other pathways. Claire O’Brien et al., “Preventable Hospitalizations among Adult Medicaid Enrollees in 2019,” Urban Institute, January 23, 2024.
Health care workers say racism in care is a major issue: 47% of U.S. health care workers said they witnessed discrimination against patients, and 52% said that racism against patients was a major problem. Employees at health facilities with a higher percentage of Black or Latino patients witnessed higher rates of discrimination. At hospitals with a majority of Black patients, 70% of workers said they witnessed discrimination against patients based on their race or ethnicity. For hospitals with mostly Latino patients, that figure was 61%. 59% of workers younger than 40 said they faced stress due to discrimination, compared with 26% of workers 60 or older. Ken Alltucker, “Nearly half of health care workers have witnessed racism, discrimination, report shows,” USA Today, 2/18/24.
Fertility treatments out of reach for the poor: A round of IVF can cost around $20,000. For comparison, the maximum allowed income for a family of two on Medicaid in New York is just over $26,000. Although Medicaid pays for about 40% of births in the United States, and 46 states and the District of Columbia have elected to extend Medicaid postpartum coverage to 12 months, fertility treatments are still not covered under Medicaid. By contrast, 45% of companies with 500 or more workers cover IVF and/or fertility drug therapy. Michelle Andrews, “If You’re Poor, Fertility Treatment Can Be Out of Reach,” KFF Health News, February 26, 2024.
Profiteers in Health Care
Medical device manufacturer reaches settlement on breathing device defects: Philips Respironics agreed to pay $479 million to settle claims that its defective continuous positive airway pressure (CPAP) devices spewed flecks of foam and gasses into the lungs of patients, causing respiratory illness and even lung cancer. More than 105,000 injuries and 385 reports of deaths that were possibly related to the foam breakdown in Philips machines have been reported to the F.D.A. Christina Jewett, “CPAP Maker Reaches $479 Million Settlement on Breathing Device Defects,” New York Times, 9/7/23.
FTC sues private equity group for attempting to create anesthesia monopoly: The firm, Welsh Carson, owns U.S. Anesthesia Partners (USAP). The firm bought competing doctor groups in its markets to gain leverage over commercial health insurers and paid shareholders large sums by saddling the company with billions of dollars in debt. As it has grown to be by far the largest anesthesia provider in Texas, it has raised prices higher than all of its competitors to match. As of early 2020, UnitedHealthcare reported that it reimbursed USAP at rates 95% higher than its in-network median for Texas and 65% higher than the Houston average. Bob Herman and Tara Bannow, “FTC sues private equity firm Welsh Carson, U.S. Anesthesia Partners for allegedly creating a monopoly,” STAT News, 9/21/23.
Columbus hospitals relieving hundreds of millions in medical debt: Four regional hospitals are relieving approximately $335 million owed by hundreds of thousands of local residents for care received between 2015-2020. Columbus residents are eligible if they earn between 200-400% of the federal poverty line, which is about $55,500-$111,000 for a family of four. This is expected to impact around 340,000 local residents, the city estimates, with the average amount forgiven coming to nearly $1,000. Tyler Buchanan, “Columbus hospitals relieving $335M in medical debt,” Axios, 10/17/23.
UnitedHealth sued over MA denials: The lawsuit alleges that United used an AI tool to deny care to beneficiaries. According to plaintiffs, Medicare Advantage members appealed less than 1% of post-acute care denials, but 90% of those denials were reversed. UnitedHealthcare cut off hospice coverage for a patient named in the lawsuit two months after his admission, deeming it medically unnecessary and denying an appeal. The patient’s family spent as much as $168,000 out of pocket for him to remain at the hospice provider until his death. Another patient had a stroke at age 74 in October 2022 and United denied coverage for 20 days of nursing home care he received, then rejected multiple appeals, the lawsuit claims. His family paid more than $70,000 as a result. Nona Tepper, “UnitedHealth sued over AI, Medicare Advantage denials,” Modern Healthcare, 11/14/23.
Profit-seekers harm patients in assisted living: More than 800,000 older Americans reside in assisted living facilities. Most residents have to pay out-of-pocket because Medicare doesn’t cover long-term care and only a fifth of facilities accept Medicaid. The industry runs operating margins around 20%, and often charges residents with extensive needs $10,000 or more a month. The national median cost of assisted living is $54,000 a year. Investigations have found that facilities have billed residents $50 per injection, $12 for a single blood pressure check, and $93 a month to order medications from a pharmacy. Jordan Rau, “Senate Probes the Cost of Assisted Living and Its Burden on American Families,” KFF Health News, 1/25/24.
Senators grill pharma CEOs on company practices: In a hearing, Senator Chris Murphy pointed out that pharmaceutical company Johnson and Johnson spent $17 billion on stock buybacks and dividends compared to $14 billion on research and development. Senator Benrie Sanders said that Bristol Meyers Squibb charges patients $7,100 per year for blood-clot drug Eliquis in the U.S., while the same product can be purchased for $900 in Canada and just $650 in France. In 2022, prices for brand-name drugs in the U.S. were at least three times higher than those in 33 other wealthy nations. Max Zahn, “Big Pharma CEOs grilled on Capitol Hill over drug prices: 4 key takeaways,” ABC News, 2/8/24.
Private equity investment in Medicare Advantage is down: In 2023, investor groups made just four MA-related deals, the lowest number since 2017. At the peak of investment in 2021, private equity groups made 19 such deals, which then declined to 12 in 2022. From 2016 to 2023 in total, private equity groups invested in 80 Medicare Advantage companies. 45 of these investments were “add-on acquisitions” in which a Medicare Advantage company was purchased by another business the investors already owned. Nona Tepper, “Private equity Medicare Advantage investment slumps: report,” Modern Healthcare, 2/13/24.
Studies and analysis of interest to single-payer advocates
“Taking Advantage: How Corporate Health Insurers Harm America’s Seniors,” Physicians for a National Health Program, May 2024. “Ultimately, the effect of enrolling in MA on the care of millions of patients is decidedly negative. The existing evidence demonstrates that MA is not doing what it promised to do, and what its participating insurers are overpaid billions to do; far from improving quality of care or outcomes, Medicare Advantage is leaving beneficiaries, health care workers, and our health care system worse off, all in the name of profit.”
“What Do Medicare Beneficiaries Value About Their Coverage?” by Gretchen Jacobson, Faith Leonard, Elizabeth Sciupac, and Robyn Rapoport, Commonwealth Fund, 2/22/24. “Delays in care resulting from prior approval requirements or unaffordable cost-sharing expenses were more likely to be reported by beneficiaries in Medicare Advantage than in traditional Medicare.”
“The burden of medical debt in the United States,” by Shameek Rakshit, Matthew Rae, Gary Claxton, Krutika Amin, and Cynthia Cox, Peterson-KFF Health System Tracker. “The SIPP survey suggests people in the United States owe at least $220 billion in medical debt. Approximately 14 million people (6% of adults) in the U.S. owe over $1,000 in medical debt and about 3 million people (1% of adults) owe medical debt of more than $10,000. While medical debt occurs across demographic groups, people with disabilities or in worse health, lower-income people, and uninsured people are more likely to have medical debt.”
“Restrictiveness of Medicare Advantage provider networks across physician specialties,” by Yevgeniy Feyman, Jose Figueroa, Melissa Garrido, Gretchen Jacobson, Michael Adelberg, and Austin Frakt, Health Services Research, 4/9/24. “Our findings suggest that rural beneficiaries may face disproportionately reduced access in these [MA] networks and that efforts to improve access should vary by specialty.”
“Older Americans Say They Feel Trapped in Medicare Advantage Plans,” by Sarah Jane Tribble, KFF Health News, 1/5/24. “Enrollment in Medicare Advantage plans has grown substantially in the past few decades, enticing more than half of all eligible people, primarily those 65 or older, with low premium costs and perks like dental and vision insurance. And as the private plans’ share of the Medicare patient pie has ballooned to 30.8 million people, so too have concerns about the insurers’ aggressive sales tactics and misleading coverage claims.”
PNHP Chapter Reports
California
In California, multiple chapters continue their work on single payer and related issues. PNHP-Ventura members have created and delivered presentations around Medicare Advantage and Medicare privatization as part of grand rounds with very positive reception. The chapter also worked on an effort to pass a Ventura City Council resolution in favor of single payer. PNHP-Humboldt members have also been presenting on MA to various senior community groups, political organizations, and local events. The chapter was even able to place ads about the dangers of MA in local newspapers. Finally, PNHP-Chico, which recently restarted activities, has been delivering informational presentations, making calls to Senators to oppose cuts to social services, and planning future events.
To get involved in California, please contact Dr. Nancy C. Greep at ncgreep@gmail.com.
Indiana

Members of Medicare for All Indiana have been hard at work together with SNaHP members passing resolutions at the Indiana State Medical Association. These resolutions include supporting Medicaid access, calling on non-profit hospitals to honor their charity care obligations, and protecting voting rights and democracy. In addition, members presented on Medicare for All at the League of Women Voters’ annual meeting in June, and gave multiple presentations on Medicare privatization throughout the year, including tabling at Farmers’ markets. The chapter also sponsored showings of American Hospitals in September.
To get involved in Indiana, please contact Dr. Rob Stone at grostone@gmail.com.
Kentucky
Members in Kentucky led a protest at Humana headquarters in downtown Louisville, demanding an end to denials of care, the right to choose your doctor, an end to forced placement in MA, and the enactment of Medicare for All. The chapter also gave several presentations and hosted webinars on value-based care, single payer, and other topics. Finally, the chapter successfully persuaded the newspaper known as the Kentucky Lantern to cover the story of Baptist Health hospitals and physicians ending contracts with Medicare Advantage companies.
To get involved in Kentucky, please contact Kay Tillow at nursenpo@aol.com.
North Carolina

In Asheville, members of Health Care for All Western North Carolina (HCFAWNC) have worked on a number of different initiatives. In October, the chapter presented to Burke County Democrats, and in November, organized a screening of the documentary “Healing US”, adding several new members to the chapter from this event. In January, members met with North Carolina House Representative Caleb Rudow to discuss single payer and his constituents’ need for it. Members also met with Senator Ted Budd to inform him of the failures of Medicare Advantage plans and to ask him not to sign the pro-MA letter.
To get involved in HCFA-WNC, please contact Terry Hash at theresamhash@gmail.com.
Washington
In Washington, members continued their tradition of holding monthly Zoom meetings with a theme and speaker. These included a report-back from four members and eight SNaHP students from around the state who attended PNHP’s 35th Anniversary Annual Meeting in Atlanta. The chapter also raised more than $20,000 in contributions for its George Martin Student Scholarship Fund, which provides support for activities of the 5 SNaHP Chapters in our region. Members worked hard to develop deeper and more productive collaboration with other organizations in the region to fight against the privatization of Medicare. These include Puget Sound Advocates for Retirement Action, Health Care for All WA, and Health Care is a Human Right WA. Finally, members have been writing and circulating sign-on resolutions, advocating for Single-Payer with state and Congressional legislators, and planning for public meetings and actions in the Spring of 2024.
To get involved in Washington, please contact Dr. David McLanahan at mcltan@comcast.net.
SNaHP Chapter Reports
Florida State University
SNaHP Students at Florida State University have focused on recruitment and collaboration. The chapter is planning to table at several student activity fairs, and has recruited members into leadership positions in the organization. Members attended a virtual town hall with Rep. Maxwell Frost in the fall, and sent students to health care focused events around Tallahassee. The chapter also continues to collaborate with other units at FSU College of Medicine on access to care for racial and ethnic minority populations. In the coming months, students will be looking to collaborate more closely with LMSA and Pride groups in the medical school.
To get involved at Florida State University, please contact Dr. Xan Nowakowski at alexandra.nowakowski@med.fsu.edu.
Hofstra University
The SNaHP chapter at the Hofstra University Zucker School of Medicine hosted a single payer 101 lecture presented by Dr. Oliver Fein in October. Students had the opportunity to learn about the basics of single payer and how it compares to our current health system in achieving affordable and universal health care coverage. Students also organized a letter writing and introduction to advocacy event. In this event, medical students learned the ins and outs of engaging in advocacy and the democratic process. These students then wrote to their state and national representatives to express support for a number of health policies, including single payer. Many students also wrote to state legislators in support of the New York Health Act.
To get involved at Hofstra University, please contact Brien Maney at bmaney1@pride.hofstra.edu.
UNC-Charlotte
Students at the undergraduate chapter of UNC-Charlotte have held several meetings on different topics. One meeting was on understanding the legislation of health care, where students heard about the legislative side of Medicare for All from Dr. George Bohmfalk and Megan Dunn. Another meeting was on reproductive justice and healthcare, held in collaboration with the UNC-Charlotte Reproductive Justice Collective to discuss how reproductive freedom relates to Medicare for All. This event was organized using information from the reproductive justice session at the PNHP Annual Meeting. The last event held was on access to mental health care, and how Medicare for All can help eliminate barriers to accessing mental health care.
To get involved at UNC-Charlotte, please contact Kayla Walker at kwalk100@uncc.edu.
University of Florida

Students at the University of Florida worked in collaboration with groups such as Medicare for All Florida and Alachua County Labor Coalition to pass a resolution in Alachua County in support of Medicare for All. The resolution passed on December 12th. The chapter also hosted 4 SNaHP events during Health Policy week for first-year medical students with local speakers and PNHP speakers Dr. Ed Weisbart, Dr. Marvin Malek, and Dr. Betty Keller. Finally, the chapter had great success with recruitment, increasing its membership from just 4 to 34 students in the last months.
To get involved at the University of Florida, please contact Patrick Haley at phaley1@ufl.edu.
Reclaiming Medicare for the Public
In late winter, legislators in the U.S. House and Senate sent a pair of letters to the Centers for Medicare and Medicaid Services, urging administrators to crack down on delays and denials in the so-called “Medicare Advantage” program—and to make sorely needed improvements to traditional Medicare. These letters were championed by Reps. Jayapal, DeLauro, and Schakowsky, and by Sens. Warren and Brown.
PNHP members were instrumental in convincing 60 Representatives and 10 Senators to sign on. We sent thousands of emails and met with dozens of legislators to talk about the dangers of Medicare profiteering.
For more information about how you can get involved with our legislative campaign, visit HealMedicare.org or email National Organizer Mandy Strenz at mandy@pnhp.org.
PNHP in the News
News items featuring PNHP members
- “Three quarters of ACOs in direct contracting model earned savings,” Healthcare Finance News, 10/24/23
- “Health care choices narrow for Kentuckians in Medicare Advantage plans,” Kentucky Commonwealth Journal, 10/25/23
- “‘This Should Be a National Scandal’: For-Profit Medicare Advantage Plans Using AI for Denials,” Common Dreams, 11/3/23
- “Physicians gather in Atlanta to march for Medicaid expansion, AMC site,” Atlanta Journal-Constitution, 11/12/23, featuring Drs. Anwar Osborne and Mindy Guo
- “Medicare Advantage Plans Disadvantage Many Elderly and Disabled People,” Truthout, 12/4/23, featuring Dr. Cheryl Kunis
- “Alachua County Commission unanimously approves resolution supporting the Medicare for All Act,” Alachua Chronicle, 12/12/23, featuring Patrick Haley
- “State lawmakers look for solutions to Georgia’s maternal mortality crisis,” Atlanta Journal-Constitution, 1/5/24, featuring Dr. Toby Terwilliger
- “Republicans Are Planning to Totally Privatize Medicare — And Fast,” Rolling Stone, 2/5/24, featuring Dr. Philip Verhoef
- “Do No Harm,” Chicago Health Magazine, 4/8/24, featuring Drs. David Ansell, Susan Rogers, and Philip Verhoef
Op-eds by PNHP members
- “Healthcare Priorities for Georgia,” by Jack Bernard, Newnan Times-Herald, 11/13/23
- “The right wing loves insurance company looting of Medicare,” by Dave Anderson, Boulder Weekly, 10/26/23
- “It’s Halloween season, and Medicare Advantage is coming as a vampire,” by Dr. Peter Gann, Evanston Roundtable, 10/30/23
- “Seniors, beware: Medicare open enrollment feels like ‘open season’ on older Americans,” by Dr. Carol Paris, The Tennessean, 10/30/23
- “Medicare Advantage is a money grab by big insurers,” by Kip Sullivan, Minnesota Reformer, 11/3/23
- “Medicare recipients should look beyond ‘benefits’ of Medicare Advantage plans,” by Dr. Jeffrey Belden, et al., Columbia Missourian, 11/6/23
- “Medicare Advantage is giving away billions to corporate insurers. It’s time we put a stop to it.” by Dr. Diljeet Singh and Rep. Pramila Jaypal, The Hill, 11/17/23
- “The siren call of Medicare Advantage,” by Dr. Robert S. Kiefner, Concord Monitor, 11/25/23
- “’Medicarelessness’ Revisited After 50 Years,” by Dr. Cheryl Kunis, MedPage Today, 11/27/23
- “Medicare Advantage is bad for patients and bad for investors,” by Dr. Philip Verhoef and Wendell Potter, STAT News, 2/28/24
- “Overpayments to Medicare Advantage costly,” by Dr. Dwight Michael, Gettysburg Times, 3/16/24
- “We need to act to rein in ‘prior authorization’,” by Dr. Marvin Malek, VTDigger, 4/18/24
- “The Path Toward Medicare for All,” by Patty Harvey, North Coast Journal, 6/6/24
Letters to the editor by PNHP members
- “Politics controls health policy from upstream,” by John Steen, VTDigger, 10/22/23
- “Medicare Advantage programs are a symptom of a sick health-care system,” by Ken Lefkowitz, Washington Post, 11/13/23
- “Medicare ‘Dis-Advantage’ plans undermine system,” by Marion Brodkey, Santa Cruz Sentinel, 11/15/23
- “Private insurers never deliver,” by Cris Currie, The Spokesman-Review, 11/17/23
- “Be wary of Medicare Advantage plans,” by Patty Harvey, The TImes-Standard, 11/23/23
- “Save Medicare from corporate profiteers,” by Leslie Nyman, Greenfield Recorder, 11/29/23
- “Medicare ‘Advantage’ is no advantage at all,” by Dr. Susanne King, The Berkshire Eagle, 12/2/23
- “Hospitals and Profits: Should They Coexist?” by Dr. Marc Lavietes, New York Times, 12/18/23
- “Letter: Medicare Advantage,” by Dr. Mary McDevitt, The Sonoma Index-Tribune, 3/7/24
The post PNHP Newsletter: Spring 2024 appeared first on PNHP.
Taking Advantage 21 May 2024 8:39 AM (10 months ago)
Physicians for a National Health Program, May 23, 2024
Table of Contents
- Executive Summary
- By the Numbers
- Introduction
- Patient Harms: Restricting Access Through Networks
- Patient Harms: Prior Authorization
- Patient Harms: Limited Coverage
- Patient Harms: Excessive Costs
- Patient Harms: Trapped in MA
- Provider Harms: Barriers to Patient Care and Administrative Burden
- Provider Harms: Corporatization of Medicine
- Conclusion
- Endnotes
- Recommended Citation
- Acknowledgements
To view a PDF version of this report, click HERE for an interactive (web-friendly) version, HERE for a printable full-color version, and HERE for a printable black & white version.
To view a one-page printable handout, click HERE for full color and HERE for black & white.
Executive Summary
Medicare Advantage (MA), the privately-administered version of Traditional Medicare (TM), is causing significant harm to America’s patients, providers, and health care system. The insurers who run MA plans claim that they lead to better patient care and outcomes while saving money, but this is far from the truth.
Patients who sign up for Medicare Advantage are forced to deal with narrow networks which heavily restrict their access to physicians and hospitals, and are often misled about the size of these networks through inaccurate listings. They must seek prior authorization for many of the tests, treatments, and other procedures ordered by their doctor, often waiting days or weeks just to be inappropriately denied approval for necessary health care. These delays can have serious consequences for a patient’s health, even sometimes resulting in death.
MA plans aggressively advertise their supplemental perks, particularly their offering of dental, vision, and hearing benefits. However, plan benefits are often highly limited and do not come close to meeting the needs of enrollees. Even worse, patients in MA who become seriously ill or develop chronic conditions end up paying thousands of dollars for their care, often struggling to afford treatment and incurring medical debt in the process. These issues often have a disproportionate impact on the most vulnerable communities, reinforcing inequities in health care access and outcomes.
When patients encounter these issues in MA and wish to switch back to Traditional Medicare, they often find that they are unable to do so. In all but four states, regulations allow insurers to deny Medigap coverage to patients who have been in MA for more than a year. Without a Medigap policy to cover additional costs, Traditional Medicare is not an affordable option for many seniors who are then forced to remain in MA despite its many flaws.
MA doesn’t just hurt patients. Physicians, nurses, and other health care workers face serious barriers to caring for patients as a result of the excessive administrative burden placed on them by MA insurers. These workers must spend hours filling out authorization forms and fighting with insurers to get necessary care approved, limiting the time they can spend on their actual jobs. MA plans also frequently delay payments for the care of enrollees, or even refuse to pay altogether, causing serious financial harm to hospitals and medical practices that have limited resources to begin with.
Medicare was created to serve the people, and MA betrays that promise. We must rein in the abuses of MA insurers, eliminate profit-seeking in Medicare and beyond, and put an end to these egregious harms.
By the Numbers
- 11.1-20.5 million: Hours per year wasted by medical practices on Medicare Advantage prior authorization requests
- 11.7 million: Number of MA beneficiaries in a “narrow network” plan that excludes more than 70% of physicians in their county, based on 2017 KFF study (i) and STAT estimate of 2024 enrollment (ii)
- 7.3 million: Number of MA beneficiaries who are underinsured based on their reporting of high health care costs, based on 2023 Commonwealth Fund study (iii) and STAT estimate of 2024 enrollment (iv)
- 36: Number of studies cited in this paper collectively finding negative outcomes for patients and providers in MA
- 2x: Increased likelihood of death after pancreatic surgery in cancer patients with MA, based on study in the Journal of Clinical Oncology (v)
Introduction
Insurance corporations in the privatized Medicare Advantage program are harming millions of America’s most vulnerable, while costing the Medicare Trust Fund tens of billions more than if those people enrolled in Traditional Medicare. These insurers force patients and health care workers alike to deal with unjustifiable prior authorization requirements, limited networks, endless denials of care, and inadequate coverage, severely disrupting care in the name of financial gain. This report will summarize, through a review of relevant academic literature, research, journalism, and original interviews conducted by PNHP, the many ways in which corporate-run Medicare harms both patients and health care workers.
Medicare Advantage, also known as MA or Medicare Part C, is a privately administered insurance program that uses a capitated payment structure, as opposed to the largely fee- for-service (FFS) structure of Traditional Medicare or TM. Instead of paying directly for the health care of beneficiaries, the federal government gives a lump sum of money to a third party (usually a commercial insurer) to “manage” patient care.
“Managed care” has promised two benefits: to save money, and to improve patient outcomes. Advocates of the insurance industry assert that private insurers, by dint of their profit incentive, will do a better job at preventing unnecessary expenses and promoting efficient spending. However, as we detailed in a previous report, MA has failed to realize any true savings, and in fact transfers tens of billions of dollars from taxpayers to corporations each year. (1) But what of the second measure? Even if Medicare Advantage is more expensive than Traditional Medicare, does it provide better care?
Insurers will tell you that the answer is a clear “yes,” using the same logic as when speaking about savings. After all, it’s taken for granted that companies must satisfy their customers in order to stay competitive and stay in business. This logic is both deceptively simple and deeply flawed. The literature comparing quality and outcomes of care between MA and TM challenges the claims of insurers. The Medicare Payment Advisory Commission (MedPAC), the most authoritative source of data and analysis on the Medicare program, has found no consistent pattern of better performance or outcomes under MA, despite its higher costs. (2) What’s more, the agency notes that the practice of “favorable selection” may skew quality and outcomes data in favor of MA. (3) By signing up less costly and thus generally healthier patients, insurers make it seem as though they do a better job of keeping patients healthy. (4) Even with this leg up, there is no persuasive evidence that MA outperforms TM on the whole. Insurers do not report much of the data that could help answer open questions about care in MA, further calling into question their claims about increased quality. (5)
Contrary to what insurers say, quality of care is often not the reason that beneficiaries enroll in an MA plan. They may be drawn in by misleading and aggressive marketing, as 17% of seniors have reported that advertisements led them to believe something about an MA plan that they later found out was not true. (6) They may sign up out of financial necessity, if they are unable to afford monthly TM premiums plus a supplemental Medigap policy. Their employer may only pay retiree benefits to an MA plan, a practice that has caused controversy around the country. (7) Or, most insidiously, they may be unhappy with their MA coverage but unable to switch to TM due to regulations detailed later in this paper. MA plans keep their customers through captive practices, not superior service. They make money not by providing the best medical services, but by withholding them. Ultimately, the effect of enrolling in MA on the care of millions of patients is decidedly negative. The existing evidence demonstrates that MA is not doing what it promised to do, and what its participating insurers are overpaid billions to do; far from improving quality of care or outcomes, Medicare Advantage is leaving beneficiaries, health care workers, and our health care system worse off, all in the name of profit.
Patient Harms: Restricting Access Through Networks
To examine the harm that MA does to patients, it is logical to begin with the act of seeking care from a physician or other provider. A key feature of Traditional Medicare, one which is both widely known and widely beloved, is that beneficiaries can access care at nearly any hospital or doctor in the country. The vast majority of practitioners and physicians in the U.S. participate in the program, and receive additional benefits to do so. (8) With TM, there are no out-of-network fees or differences in payments between providers. This is not the case in MA.
Medicare Advantage insurers employ networks just the same as nearly any other commercial insurance policy. Over half of MA plans are health maintenance organizations (HMOs), which tend to be more restrictive than other plans, featuring smaller networks, little out-of-network coverage, and referral requirements for specialist care. (9) These HMOs also enroll the greatest number of MA beneficiaries–around 62% of the total beneficiary population based on estimates from 2021. (10)
For most insurance plans, the ostensible goal of establishing a network is to negotiate lower payment rates with a smaller set of providers. (11) However, when it comes to MA, payment rates are largely set near or at those of Traditional Medicare, so rate negotiations are less of an incentive. Instead, narrow networks are formed with health systems that have lower utilization rates, as a means of saving money for the insurer. (12) In addition, insurers try to form networks using providers who can help them to achieve high star ratings in MA’s quality bonus program, as the ensuing reimbursement bonuses translate into extra profits for the insurer. (13) It is worth noting that the quality bonus program itself is highly flawed, and high star rating plans do not necessarily deliver better care to MA beneficiaries. (14)
The consequence of these financial incentives is that narrow physician networks are very common in Medicare Advantage. A study from KFF found that a little over one in three MA plans (35%) had a “narrow” physician network, meaning one that excluded more than 70% of physicians in a given county. (15) A further 43% of plans had “medium” networks, with anywhere from 30-69% of physicians included.
Only 22% of plans had “broad” networks that included more than 70% of physicians in the county area. On average, plans excluded over half of physicians in a county. (16) Although percentages of narrow networks for hospitals are lower, on average MA plans still only cover just over half (51%) of hospitals in a county. (17) Predictably, MA insurers often fail to meet the network adequacy standards that are set for them by the Centers for Medicare and Medicaid Services (CMS). (18)
These narrow networks persist across a variety of different specialties and categories of care. Multiple studies have found that psychiatrists are some of the most heavily restricted specialists in MA networks, with nearly two-thirds of plans covering less than 25% of psychiatrists in the network service area. (19) According to KFF’s physician study, 36% of assessed plans were even more narrow, with less than 10% of psychiatrists in the county included. (20) KFF also found that close to one-fifth of MA plans included less than five cardiothoracic surgeons, less than five neurosurgeons, less than five plastic surgeons, and less than five radiation oncologists. (21)
Evidence shows that patient demographics affect network size as well. Physicians who care for the greatest number of patients who are dual-eligible for Medicare and Medicaid (meaning patients who are both elderly/disabled and also struggling financially) have been found to have a lower chance of being included in MA plan networks. (22) The same is true for physicians who treat patients with higher levels of medical risk, which tracks with indications that MA plans actively seek to avoid such patients. (23) Patients in rural areas are also more likely to face restrictive networks across a number of specialties. (24)
Narrow networks compromise access to the best quality of care for the sickest individuals. Cancer care, already a nightmare to navigate for anyone regardless of their insurance, is especially bad for MA patients in terms of network inclusion. MA patients are much less likely than TM patients to be able to access cancer care at teaching hospitals, Commission on Cancer-accredited hospitals, or National Cancer Institute-designated centers. (25) MA patients are also less likely to have access to high-volume hospitals with more experience doing complex, high-risk surgery for cancers of the lung, esophagus, stomach, liver, pancreas, or rectum. This lack of access, largely a result of narrow networks as well as delays in receiving care, was found to have likely contributed to higher 30-day mortality rates for liver, pancreas, and stomach cancer surgeries. In other words, narrow networks are killing cancer patients. (26)
A final issue with MA networks is the prevalence of “ghost” networks. These networks claim to include providers who are not actually in the network, and sometimes no longer even exist. A study by the U.S. Senate Committee on Finance found that over 80% of identified listings for mental health providers in studied MA plans were inaccurate or unavailable. Of 120 provider listings who were contacted, researchers only succeeded in setting up an appointment with 22. (27)
Another study of dermatologists in MA networks found that more than half of the dermatologists listed had incorrect contact information, were deceased, retired, had moved, were not accepting new patients, did not accept the insurance plan, or were subspecialized. (28) Ghost networks present a huge transparency issue for MA beneficiaries, who may select a plan based on the appearance of a robust network only to find there are far fewer available providers than initially shown.
It is also worth noting that hospital networks in MA may be shrinking as health systems continue to opt out of accepting Medicare Advantage due to low reimbursement rates and the administrative burden of insurer practices like prior authorization. Dozens of hospitals, including large and well-known systems like Scripps Health and Mayo Clinic, have indicated that they will no longer take most or all MA plans because of these issues. (29) Patients, especially those in rural areas or places with few options for medical care, suffer greatly from these closures, which further decrease access to care for everyone in the community. (30)
Patient Narrative: Restricting Cancer Care
“In 2021, my wife became very seriously ill very suddenly, within a matter of 3 or 4 days, and she was diagnosed on the 5th or 6th day with category 4 brain cancer, glioblastoma, inoperable. Pretty much from that point in time, it was always a fight with insurance. Which hospital could we be in? Could we coordinate benefits between hospitals? Some services might only be covered in one hospital and other services in another hospital. What kind of treatment could she get approved for as she got progressively worse? Would she be able to be admitted to hospice? I wouldn’t wish it on anybody. It was absolutely horrible.” – Husband of MA patient, New York
Patient Narrative: Restrictive Networks
“Trying to find a dentist on my Blue Cross plan was virtually impossible. They were not accepting new patients, at least not when I told them I was a Medicare Advantage patient. After a lot of searching, I finally found a dentist, and now, what I have to do is take a ferry from my home, then drive about 20 miles into another town, and there is the only dentist I can go to. All of the travel combined takes about an hour to an hour and a half each way, when there are dentists who won’t accept Medicare Advantage patients ten minutes from my house.” – MA patient, Washington
Provider Narrative: Ghost Networks
“When Medicare Advantage plans were taking off in our area some years ago, Coventry Health, which later became a part of Aetna, sold a Medicare Advantage plan in the area that listed us as a network provider—but we weren’t. The first patient that showed up with this plan, I had to look it up and tell them we weren’t in-network, and they were furious, because this plan was sold to them on this presumption. This was bad enough and they sold this plan to enough people that I reported them to CMS for contracting issues, and they had to change their network.” – Primary care practice office manager, Missouri
Patient Harms: Prior Authorization
Even if patients are able to obtain an appointment, the challenges do not end there. Like other insurance plans, MA plans practice “utilization management,” requiring prior authorization (PA) for most tests, procedures, and medications. Ostensibly, the purpose of this practice is to prevent unnecessary use of medical services; in practice, it is often a way for insurers to delay paying for necessary care in the hopes that patients will abandon their efforts to receive it. By contrast, beneficiaries in Traditional Medicare are only required to obtain prior authorization for a small set of services, meaning delays in care due to denial are much rarer.
When it comes to its effect on patient care, prior authorization is almost universally hated by health care providers. A survey of physicians conducted in 2022 by the American Medical Association (AMA) found that 94% of physicians reported that PA caused delays in care for their patients, with 80% saying that this delay led to treatment abandonment at least some of the time. (31) 89% of physicians said that PA has a negative effect on patient treatment, with 25% of physicians even reporting that delays in treatment due to PA led to a patient’s hospitalization. (32) Although the AMA’s survey was about PA in general and not specific to PA in Medicare Advantage, the organization cited this data in an open letter to the Centers for Medicare and Medicaid Services (CMS) calling for the agency to crack down on the abuse of PA in the MA program. (33)
Many problems have been reported with the use of prior authorization in Medicare Advantage. According to KFF, in 2021, more than 35 million prior authorization requests were submitted to MA plans, of which about 2 million or 6% were fully or partially denied. (34) It is important to remember that these denials do not account for delays in approval, which can take weeks and still result in profound negative consequences for patients (nor do these statistics reflect the number of requests physicians never submit because of the anticipated hassle of approval). The appeal process for denied requests also demonstrates the true harm of this process: just 11% of the 2 million denied requests were appealed, but in those appeals, 82% of denials were overturned. (35) These findings were echoed in a report by the U.S. Department of Health and Human Services’ (HHS) Office of the Inspector General (OIG), which found that from 2014-2016, just 1% of payment or service denials in Medicare Advantage Organizations (MAOs) were appealed, but 75% of appeals overturned the initial decision. (36)
In effect, these statistics suggest that denials are often entirely arbitrary, as even one attempt to question their use results in the request’s approval in the vast majority of cases. The inpatient denial rate in MA is also higher than in other programs, with a survey by the American Hospital Association (AHA) finding that 19.1% of inpatient prior authorization requests in MA were denied, compared with 15.5% for Medicaid Managed Care patients and 11.4% for commercial insurance patients. (37) Here, too, the overturn rate on appeal was high, with 69% of MA appeals resulting in a reversal of the initial decision. (38)
Indeed, studies and reporting have demonstrated some of the magnitude and characteristics of inappropriate denials in MA. Despite statutory requirements for MA to cover all the same services as TM (and consistent claims by CMS and insurers that plans do so), an HHS OIG report from 2022 found that 13% of denials in MA, close to 1 in 7, would have been approved in TM. (39) 18% of denied requests, or close to 1 in 5, met both Medicare coverage rules and MA billing rules, meaning their denial was most charitably the result of human or system error. (40) An investigation by STAT News revealed that, contrary to claims of careful review by medical experts, insurers were using unregulated AI algorithms designed to cut off care as soon as possible based on training data, without adequate regard for the individual circumstances of the patient. (41) Another STAT investigation also revealed that the insurer UnitedHealth developed secret criteria used to deny care to patients in rehabilitation care without explanation. (42)
MA beneficiaries are aware of and concerned by the excessive delays and denials of their care as a result of prior authorization. A survey by the Commonwealth Fund found that 22% of patients on MA reported delays in care due to need for approval, compared with just 13% of TM patients. (43)
Provider Narrative: Prior Authorization
“I had a patient with several chronic diseases who was very sick and had just survived major abdominal surgery, almost miraculously. In the aftermath, she desperately needed to go to acute rehab, which is the most intensive rehab – we found a facility, she liked it, her family liked it, and then her MA plan looked at the place and said ‘No, she’s healthy enough to not go to acute rehab, we won’t authorize it.’ This was after our PM&R specialist, physical therapist, and 3 MDs on our team had told her she needed acute rehab, and that it was the only thing that would keep her out of the hospital again. And this insurer, without anyone ever looking at her, rejected that conclusion. And we knew that on Traditional Medicare this never would’ve happened.” – Internal medicine resident, Illinois
Patient Harms: Limited Coverage
Besides delaying and denying care through prior authorization, MA plans also explicitly restrict care ahead of time via the use of limits on benefits and coverage. These restrictions may, for example, set an upper bound on the number of days a patient can be admitted for an inpatient treatment, or determine what drugs will be included on a formulary.
Medicare Advantage insurers are known for aggressively advertising “supplemental benefits” such as dental, vision, and hearing. These benefits are not covered by Traditional Medicare, and thus patients on TM generally require supplemental coverage to access these services. An analysis of MA television ads found that 92% mentioned supplemental benefits as a perk of the plans, compared with just 22% touting better access to physicians. (44) What these ads fail to describe are the significant limits applied to these benefits.
59% of enrollees in an MA plan with dental coverage have a maximum benefit of $1,000 or less, beyond which any dental services will not be covered. (45) This is despite the fact that 19% of Medicare beneficiaries have reported spending more than $1,000 on dental care in out-of-pocket costs during a yearlong period. (46) Hearing services in MA are similarly restricted, as 91% of beneficiaries with hearing coverage face limits on the number of hearing aids they can receive in a given time period. (47) 32% of beneficiaries with hearing coverage have both frequency limits and a dollar limit applied to their benefit. (48) The average dollar limit for hearing coverage is $960, despite the fact that an average pair of prescription hearing aids costs over $4,000. (49) The dollar limits for vision coverage in MA are perhaps the most striking; 99% of beneficiaries receiving vision benefits have a dollar limit on coverage, and the average limit is just $160 per year. (50)
Similar coverage restrictions are present in other aspects of care as well. About 60% of MA enrollees are in plans that do not cover out-of-network outpatient mental health or substance use disorder services, with a similar number of enrollees in plans that do not cover out-of-network mental health hospitalization or opioid treatment programs. (51) A study of prescription drug coverage among 4 large MA insurers found that of the 20 most common physician-administered drugs, 17 were subject to prior authorization and 10 were subject to step therapy by at least 1 insurer (step therapy refers to a practice wherein insurers require the use of alternative treatments, and only approve the requested treatment if those prove unsuccessful). (52)
Over the period from 2018 to 2020, many of these drugs were also removed from all 4 MA- Part D (MA-PD) insurer formularies, meaning they would no longer be covered at all. Humana, for example, covered 14 of the 20 listed drugs on its Part D formulary in 2018, but by 2020 only included 4 of them. (53)
Patient Narrative: Limited Coverage
“My grandfather, who has pancreatic cancer, has to pay thousands of dollars before he gets any real coverage. On top of that, he has copays and coinsurance he needs to pay as well. He even has had to pay out-of-pocket fees for emergency life flights he needed due to complications from his chemotherapy. I know those would’ve been covered fully under Traditional Medicare.” – Grandson of MA patient, Pennsylvania
Patient Harms: Excessive Costs
Even with insurance, cost-sharing for medical services is virtually unavoidable in the United States. Traditional Medicare, for all its benefits, generally covers only 80% of the cost for outpatient services, leaving patients responsible for the other 20% (usually covered by a Medigap plan). (54) However, cost-sharing in Medicare Advantage plans is often egregious, and can lead to serious affordability issues for beneficiaries.
In a survey conducted by the Commonwealth Fund, 22% of seniors on MA reported high health care costs in the previous year, compared with 13% of seniors on TM with a Medigap supplement. (55) 41% of MA enrollees said they had problems accessing care because of high costs, compared with 35% of those in Traditional Medicare plus Medigap. Finally, 21% of those on MA reported problems paying off medical bills or debt, compared to 14% of those on TM plus Medigap. (56) Another survey from KFF found that across white, Hispanic, and Black racial groups, higher percentages of beneficiaries reported cost-related problems in MA compared to TM with a Medigap supplement. The biggest difference was among Black beneficiaries; 32% reported cost-related problems on MA, while just 20% reported the same on TM with Medigap. (57) These gaps increased for beneficiaries reported to be in fair or poor health, lending more credence to the idea that MA is especially bad for those actively dealing with significant health issues. (58)
Patient Narrative: Excessive Costs
“Like a lot of people, I thought Medicare Advantage was cheaper, and it’s supposed to cover everything Medicare covers, right? That’s the way it’s supposed to work. I made the mistake of choosing a UnitedHealth MA plan, and it was about a year later I realized what kind of hell I was in when I ended up inpatient. I was looking at $300+ dollars a night bills for being inpatient. And because of my health issues, I was ending up in the hospital nearly every six weeks, staying for a few days to a week and then coming out with these monstrous bills. As long as you’re not sick, Medicare Advantage is great – you’re spending less money! But when you do get sick, the co-pays, the co-insurance, out of pocket costs, they grow so fast, and you never hit the deductible.” – MA patient, New Hampshire
Patient Harms: Trapped in MA
One of the promises of free-market advocates in health care is the idea of “consumer choice.” The insurance industry will claim that the availability of a wide variety of plans allows beneficiaries to find one that suits their personal needs, and encourages competition among insurers that leads to better policies. However, this narrative elides the serious problems MA enrollees face in leaving the program if they find it unsuitable.
There is substantial evidence that many patients, especially those who are more ill or face high medical costs, tend to leave MA at high rates. A report by the Government Accountability Office (GAO) found that Medicare beneficiaries in their last year of life (when medical costs are generally very high) disenroll from MA back to TM at more than twice the rate of all other beneficiaries. (59) A similar study in Health Affairs found that the switching rates from MA to TM were generally higher than rates for the reverse among patients receiving high-cost services like long-term nursing home care (17% vs 3%), short-term nursing home care (9% vs 4%), and home health care (8% vs 3%). (60)
Not all enrollees have the option of leaving MA when things go wrong, though. When beneficiaries first become eligible for Medicare, they have the option of signing up for MA or TM. For their first six months of eligibility, these beneficiaries are protected by “guaranteed issue” requirements for supplemental Medigap plans. This means that Medigap insurers are not allowed to deny any senior a Medigap policy, nor can they engage in “medical underwriting” to potentially charge a higher premium based on health history or other factors. (61) This six month period is extended to twelve months when a beneficiary joins MA.
However, once this period is up, these protections disappear in all but four states. If an enrollee outside of these states signs up for MA during their initial open enrollment period, and then decides to switch to TM during the next year’s open enrollment period, they are no longer guaranteed to receive a Medigap policy, and can be denied on the basis of their medical history. Many seniors are unable to afford the 20% of costs covered by Medigap, meaning their only option is to stick with MA, even if they are unhappy with their coverage. (62) While more states do require “community rating,” wherein insurers must charge all recipients of a Medigap plan the same premiums, these protections mean little to those who are outright denied coverage to begin with. (63) Thus, MA plans get to keep many of their customers not on the basis of their high- quality services, but because they simply have nowhere else to go.
Patient Narrative: Trapped in MA
“If my husband gets older and develops more serious problems, his access to a specialist may be restricted under his MA plan. So we would like to pull him out and get him on Traditional Medicare, and my worry is that now he’s being upcoded, he has a high risk health profile, so how much is Medigap going to cost if we can get it? Who knows about these kinds of problems until later on?” – Wife of MA patient, North Carolina
Provider Harms: Barriers to Patient Care and Administrative Burden
Thus far, we have discussed the myriad harms that MA inflicts upon patients. It is worth remembering, however, that MA is not only a problem for them. Medicare Advantage makes the jobs of physicians and health care workers substantially more difficult, contributing to stress, burnout, and moral injury, which refers to the psychological impacts of working in a system that forces providers to compromise their ethical commitment to patients due to the profit-driven nature of the health care system. (64)
As discussed earlier, limited networks and prior authorization are two techniques used by MA insurers to deprive patients of care as a means of saving money. Physicians are forced to contend with these practices daily, greatly hampering their ability to adequately care for patients. Limitations in networks mean that physicians often cannot refer patients to their preferred specialist or one that is convenient to the patient, making it harder to follow through on treatment plans and increasing the odds that patients will abandon treatment. These failures in treatment can weigh heavily on physicians, especially when they result in harm to a patient’s health.
Even if patients are able to get an appointment and receive a diagnosis, the physician will often need to spend hours wrestling with the insurer to justify their desired course of action and receive prior authorization for it. These interactions can be highly frustrating; in the previously mentioned survey by the AMA, 31% of physicians reported that PA criteria rarely or never follow evidence-based guidelines approved by medical specialty societies. (65) In other words, many physicians believe that insurers are denying care based on faulty premises, rejecting the expertise of these physicians and established national guidelines in favor of their own dubious standards.
The administrative burdens of prior authorization are significant. 88% of physicians describe the burden of PA as high or extremely high. (66) 35% of physicians surveyed reported that they have needed to hire staff members to work exclusively on prior authorization. (67)
In a survey of practices conducted by the Medical Group Management Association (MGMA), groups were asked to name the type of policy most burdensome for obtaining prior authorization: 46% of groups said Medicare Advantage, compared with 32% naming commercial plans and just 4% naming Traditional Medicare. (68) 84% of practices also reported that PA requirements for MA had increased in the last 12 months. (69) When asked if the clinician hired by the insurer to review an authorization held relevant expertise to the treatment in question, 72% of groups said they did not. (70) And perhaps most strikingly, an overwhelming 97% of practices said their patients had experienced delays and denials of necessary care due to prior authorization. (71)
The AMA’s physician survey found that practices spend an average of 14 hours each week processing 45 prior authorization requests, for a mean time of about 19 minutes per request. (72) Taking this figure as a global average (keeping in mind that practices rate prior authorization in MA as more burdensome than other types), the 35 million requests KFF reported were made in 2021 would result in roughly 11.1 million hours spent just on prior authorization for Medicare Advantage. Using a higher reported average time of 35 minutes per request from the MGMA survey, this number increases to 20.5 million hours. That is just over 1200 years at a minimum, and over 2300 years at maximum–or, in health care terms, anywhere from 35 to 65 million average patient visits. (73)
Prior authorization is not the only aspect of MA that results in administrative burden to physicians. In another survey from the MGMA, roughly 86% of medical group practices reported MA chart audits as being at least moderately burdensome to the practice, with 62% reporting that audits were very or extremely burdensome. (74) Because these chart audits are often used by MA insurers to inappropriately extract more money from the Medicare fund via upcoding, this also means that physicians are incurring a significant time and resource burden for the financial benefit of insurers. This is yet another example of MA contributing to moral injury among physicians. (75)
Provider Narrative: Barriers to Patient Care
“We had a patient recommended for acute rehab. He was medically ready, but insurance denied him. We had to do an appeal, and we’re waiting on the results of the appeal, but he’s been here for 20 days, and 10 of those days have been us fighting with the insurance. In that time he’s developed pneumonia.” – Nurse and case manager, Illinois
Provider Narrative: Administrative Burden
“In one month, the staff for our two oncologists did 360 prior authorizations for their patient population–so much so that I’ve had to add another full-time equivalent employee just to do prior authorizations in the oncology unit. And every request in there is urgent.” – CEO of health system, Connecticut
Provider Harms: Corporatization of Medicine
In a general sense, physicians are increasingly under the thumb of large corporations or other entities that interfere with the practice of medicine. Approximately 74% of physicians are now employed by a hospital, health system, health insurer, private equity firm, or other corporate entity. Over a three year period from 2019-2021, the percentage of corporate-owned medical practices increased an astonishing 39%. (76) In 30% of metropolitan statistical areas (MSAs) in the United States, one private equity firm owned more than 30% of physician practices in a given specialty; in 13% of MSAs, one private equity firm owned more than 50% of practices. (77)
One significant motive for this rapid increase in corporate control of medicine is the massive profit machine that is Medicare Advantage. (78) Health insurers and private equity groups seek to control providers, encouraging them to upcode diagnoses and carefully managing the amount of care that their employees are allowed to give to beneficiaries. In one reported instance, the combined health system and insurer Kaiser Permanente called physicians during lunch breaks and after work to ask them to add more diagnoses to the charts of their patients, even offering bonuses and bottles of champagne as a reward for doing so. (79)
Another method of compelling doctors to participate in the financialization of care is through the use of “full-risk” or “global risk” models, in which physicians assume the financial risk of caring for patients and only make money if they can stay under a certain budget. MA plans have increasingly adopted such models in contracts with physician groups and health systems, leading some to fear that doctors will have to decide between providing the necessary amount of care for a patient, or meeting their budget in order to stay afloat. (80)
By placing financial concerns in the hands of physicians, MA plans subject them to moral injury. To consider profit in the determination of a patient’s care goes against the most important ethical standards that health care providers set for themselves; however, the reality is that physicians in the United States must already do this as a result of the constraints placed upon them by insurers like those in Medicare Advantage. When a physician has to prescribe a less effective medication because it is the only one covered by the patient’s plan, or when a patient must wait 3 months for a surgery that will allow them to walk without pain, profit motives have already infected the standard of care. The overt corporatization of medicine and the placing of financial incentives explicitly into the hands of physicians are simply the next logical steps in this process.
Provider Narrative: Corporatization of Medicine
“My patient was told by an MA plan that they would no longer cover a particular calcium channel blocker, and that the patient needed to be on a different one. The cost difference here could not have been significant, but they switched the coverage, and encouraged the patient to get their drugs by mail. In the wake of all this shuffling around without my involvement, the patient got confused, and was taking both medications. They came in profoundly hypotensive, and we had to keep them on IV fluids all day to avoid a hospitalization. All this came from the effort of trying to pinch a penny, but what I really noticed was this was a pulling apart of what is most important in medicine – the doctor-patient relationship, and the pharmacist-patient relationship. It was all about the dollar.” – Primary care physician, South Carolina
Conclusion
Medicare Advantage represents the worst of private insurance coming to take over the best system of health care that America has to offer. Insurers in MA prey on some of the most vulnerable among us, luring them in with false promises of superior coverage and low costs only to make every effort possible to prevent them from accessing necessary health care, all while siphoning billions of dollars from taxpayers. The more MA is allowed to expand, the more harm will come to patients, physicians, hospitals, and the health care system writ large. More patients will die waiting for care to be approved, more doctors will face tremendous burdens trying to prevent this outcome, and more hospitals in areas of critical need will close as MA plans refuse to pay for their services.
The money that goes to profit-driven insurers in MA should instead be used to improve Traditional Medicare, including by adding dental, vision, and hearing coverage as well as establishing an out-of-pocket spending cap. Traditional Medicare follows the original spirit of the program, one that was created to serve all Americans without the perverse incentives that come from a profit motive. This is the model we should be following in our health system, instead of devoting more dollars to the failed experiments of managed care. We must eliminate out-of-control profit seeking in Medicare and beyond, both by reining in the abuses of insurers via executive action and legislation, and by greatly expanding our public health insurance programs. It’s time to take Medicare back for the people.
Endnotes
- PNHP, “Our Payments, Their Profits,” October 2023, https://pnhp.org/system/assets/uploads/2024/01/MAOverpaymentReport_Oct2023.pdf.
- MedPAC, “Report to the Congress: Medicare Payment Policy,” March 2023, https://www.medpac.gov/wp-content/uploads/2023/03/Mar23_MedPAC_Report_To_Congress_SEC.pdf, 367.
- Ibid., 366.
- Ibid.
- Elizabeth Warren et al., “Letter to Admin Brooks-LaSure Re: MA Data,” December 7, 2023, https://www.warren.senate.gov/imo/media/doc/2023.12.07%20Letter%20to%20Admin.%20Brooks-LaSure%20re%20MA%20Data.pdf.
- Gretchen Jacobson et al., “The Private Plan Pitch: Seniors’ Experiences with Medicare Marketing and Advertising,” Commonwealth Fund, September 12, 2023, https://www.commonwealthfund.org/publications/issue-briefs/2023/sep/private-plan-pitch-seniors-experiences-medicare-marketing-advertising.
- Chris Sommerfeldt, “Retired NYC workers sue to block Mayor Adams’ latest Medicare Advantage Plan,” New York Daily News, May 31, 2023, https://www.nydailynews.com/2023/05/31/retired-nyc-workers-sue-to-block-mayor-adams-latest-medicare-advantage-plan-exclusive/.
- Nancy Ochieng and Gabrielle Clerveau, “How Many Physicians Have Opted Out of the Medicare Program?” KFF, September 11, 2023, https://www.kff.org/medicare/issue-brief/how-many-physicians-have-opted-out-of-the-medicare-program/.
- Meredith Freed et al., “Medicare Advantage 2024 Spotlight: First Look,” KFF, November 15, 2023, https://www.kff.org/medicare/issue-brief/medicare-advantage-2024-spotlight-first-look/.
- “Medicare Data Hub: Medicare Advantage,” Commonwealth Fund, https://www.commonwealthfund.org/medicare-data-hub/medicare-advantage.
- Andréa Elizabeth Caballero et al., “Are Limited Networks What We Hope And Think They Are?” Health Affairs, February 12, 2018, https://www.healthaffairs.org/content/forefront/limited-networks-we-hope-and-think-they.
- Laura Skopec et al., “Why Do Medicare Advantage Plans Have Narrow Networks?” Urban Institute, November 2018, https://www.urban.org/sites/default/files/publication/99414/why_do_medicare_advantage_plans_have_narrow_networks.pdf, 5.
- Ibid., 5-7.
- Laura Skopec and Robert A. Berenson, “The Medicare Advantage Quality Bonus Program: High Cost for Uncertain Gain,” Urban Institute, June 26, 2023, https://www.urban.org/research/publication/medicare-advantage-quality-bonus-program.
- Gretchen Jacobson et al., “Medicare Advantage: How Robust Are Plans’ Physician Networks?” KFF, October 5, 2017, https://www.kff.org/medicare/report/medicare-advantage-how-robust-are-plans-physician-networks/.
- Ibid.
- Gretchen Jacobson et al., “Medicare Advantage Hospital Networks: How Much Do They Vary?” KFF, June 20, 2016, https://www.kff.org/medicare/report/medicare-advantage-hospital-networks-how-much-do-they-vary/.
- Eric Krupa, “Voices of Medicare: Medicare Advantage Network Inadequacy,” Center for Medicare Advocacy, https://medicareadvocacy.org/voices-of-medicare-medicare-advantage-network-inadequacy/.
- Jane M. Zhu et al., “Psychiatrist Networks In Medicare Advantage Plans Are Substantially Narrower Than In Medicaid And ACA Markets,” Health Affairs, July 2023, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2022.01547?journalCode=hlthaff.
- Jacobson et al., “Medicare Advantage Hospital Networks,” https://www.kff.org/medicare/report/medicare-advantage-how-robust-are-plans-physician-networks/.
- Ibid.
- Jung Ho Gong et al., “Proportion of Physicians Who Treat Patients With Greater Social and Clinical Risk and Physician Inclusion in Medicare Advantage Networks,” JAMA Health Forum, July 21, 2023, https://jamanetwork.com/journals/jama-health-forum/fullarticle/2807454.
- Ibid.
- Yevgeniy Feyman et al., “Restrictiveness of Medicare Advantage provider networks across physician specialties,” Health Services Research, April 9, 2024, https://pubmed.ncbi.nlm.nih.gov/38594081/.
- Mustafa Raoof et al., “Medicare Advantage: A Disadvantage for Complex Cancer Surgery Patients,” Journal of Clinical Oncology, November 10, 2022, https://ascopubs.org/doi/full/10.1200/JCO.21.01359.
- Ibid.
- Senate Committee on Finance, “Medicare Advantage Plan Directories Haunted by Ghost Networks,” May 3, 2023, https://www.finance.senate.gov/imo/media/doc/050323%20Ghost%20Network%20Hearing%20-%20Secret%20Shopper%20Study%20Report.pdf, 3.
- Jack S. Resneck Jr. et al., “The accuracy of dermatology network physician directories posted by Medicare Advantage health plans in an era of narrow networks,” JAMA Dermatology, December 2014, https://pubmed.ncbi.nlm.nih.gov/25354035/.
- Claire Wallace, “8 health systems calling it quits with Medicare Advantage: What ASCs should know,” Becker’s ASC Review, September 26, 2023, https://www.beckersasc.com/asc-coding-billing-and-collections/8-health-systems-calling-it-quits-with-medicare-advantage-what-ascs-should-know.html.
- Sarah Jane Tribble, “Tiny, Rural Hospitals Feel the Pinch as Medicare Advantage Plans Grow,” KFF Health News, October 23, 2023, https://kffhealthnews.org/news/article/medicare-advantage-rural-hospitals-financial-pinch/.
- American Medical Association, “2022 AMA prior authorization (PA) physician survey,” https://www.ama-assn.org/system/files/prior-authorization-survey.pdf.
- Ibid.
- American Medical Association et al., “Open Letter to Chiquita-Brooks LaSure,” February 13, 2023, https://searchlf.ama-assn.org/letter/documentDownload?uri=%2Funstructured%2Fbinary%2Fletter%2FLETTERS%2FPA-sign-on-letter-Part-C-and-D-rule.zip%2FPA-sign-on-letter-Part-C-and-D-rule.pdf.
- Jeannie Fugelsten Biniek and Nolan Sroczynski, “Over 35 Million Prior Authorization Requests Were Submitted to Medicare Advantage Plans in 2021,” KFF, February 2, 2023, https://www.kff.org/medicare/issue-brief/over-35-million-prior-authorization-requests-were-submitted-to-medicare-advantage-plans-in-2021/.
- Ibid.
- U.S. Department of Health and Human Services Office of Inspector General, “Medicare Advantage Appeal Outcomes and Audit Findings Raise Concerns About Service and Payment Denials,” September 2018, https://oig.hhs.gov/oei/reports/oei-09-16-00410.pdf.
- American Hospital Association, “Addressing Commercial Health Plan Challenges to Ensure Fair Coverage for Patients and Providers,” November 2022, https://www.aha.org/system/files/media/file/2022/10/Addressing-Commercial-Health-Plan-Challenges-to-Ensure-Fair-Coverage-for-Patients-and-Providers.pdf, 12.
- Ibid.
- U.S. Department of Health and Human Services Office of Inspector General, “Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care,” April 2022, https://oig.hhs.gov/oei/reports/OEI-09-18-00260.pdf.
- Ibid.
- Casey Ross and Bob Herman, “Denied by AI: How Medicare Advantage plans use algorithms to cut off care for seniors in need,” STAT News, March 13, 2023, https://www.statnews.com/2023/03/13/medicare-advantage-plans-denial-artificial-intelligence/.
- Bob Herman and Casey Ross, “UnitedHealth used secret rules to restrict rehab care for seriously ill Medicare Advantage patients,” STAT News, December 28, 2023, https://www.statnews.com/2023/12/28/medicare-advantage-united-health-navihealth-rehab-care-restrictions/.
- Gretchen Jacobson et al., “What Do Medicare Beneficiaries Value About Their Coverage?” Commonwealth Fund, February 22, 2024, https://www.commonwealthfund.org/publications/surveys/2024/feb/what-do-medicare-beneficiaries-value-about-their-coverage.
- Jeannie Fuglesten Biniek et al., “How Health Insurers and Brokers Are Marketing Medicare,” KFF, September 20, 2023, https://www.kff.org/report-section/how-health-insurers-and-brokers-are-marketing-medicare-report/#miss-out-on-benefits.
- Meredith Freed et al., “Dental, Hearing, and Vision Costs and Coverage Among Medicare Beneficiaries in Traditional Medicare and Medicare Advantage,” KFF, September 12, 2021, https://www.kff.org/health-costs/issue-brief/dental-hearing-and-vision-costs-and-coverage-among-medicare-beneficiaries-in-traditional-medicare-and-medicare-advantage/.
- Meredith Freed et al., “Drilling Down on Dental Coverage and Costs for Medicare Beneficiaries,” KFF, March 13, 2019, https://www.kff.org/medicare/issue-brief/drilling-down-on-dental-coverage-and-costs-for-medicare-beneficiaries/.
- Meredith Freed et al., “Dental, Hearing, and Vision Costs and Coverage Among Medicare Beneficiaries in Traditional Medicare and Medicare Advantage.”
- Ibid.
- Tom Horton, “How much do hearing aids cost?” CBS News, April 26, 2024, https://www.cbsnews.com/essentials/how-much-do-hearing-aids-cost/.
- Ibid.
- Meredith Freed et al., “Mental Health and Substance Use Disorder Coverage in Medicare Advantage Plans,” KFF, April 28, 2023, https://www.kff.org/mental-health/issue-brief/mental-health-and-substance-use-disorder-coverage-in-medicare-advantage-plans/.
- Kelly E. Anderson and G. Caleb Alexander, “Medicare Advantage Coverage Restrictions for the Costliest Physician-Administered Drugs,” American Journal of Managed Care, July 12, 2022, https://www.ajmc.com/view/medicare-advantage-coverage-restrictions-for-the-costliest-physician-administered-drugs.
- Ibid.
- Center for Medicare Advocacy, “Part B,” https://medicareadvocacy.org/medicare-info/medicare-part-b/.
- Faith Leonard et al., “Medicare’s Affordability Problem: A Look at the Cost Burdens Faced by Older Enrollees,” Commonwealth Fund, September 19, 2023, https://www.commonwealthfund.org/publications/issue-briefs/2023/sep/medicare-affordability-problem-cost-burdens-biennial.
- Ibid.
- Jeannie Fuglesten Biniek et al., “Cost-Related Problems Are Less Common Among Beneficiaries in Traditional Medicare Than in Medicare Advantage, Mainly Due to Supplemental Coverage,” KFF, June 25, 2021, https://www.kff.org/medicare/issue-brief/cost-related-problems-are-less-common-among-beneficiaries-in-traditional-medicare-than-in-medicare-advantage-mainly-due-to-supplemental-coverage/.
- Ibid.
- Government Accountability Office, “Beneficiary Disenrollments to Fee-for-Service in Last Year of Life Increase Medicare Spending,” June 2021, https://www.gao.gov/assets/gao-21-482.pdf.
- Momotazur Rahman et al., “High-Cost Patients Had Substantial Rates Of Leaving Medicare Advantage And Joining Traditional Medicare,” Health Affairs, October 2015, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2015.0272?journalCode=hlthaff.
- Centers for Medicare and Medicaid Services, “Get ready to buy,” https://www.medicare.gov/health-drug-plans/medigap/ready-to-buy.
- Sarah Jane Tribble, “Older Americans Say They Feel Trapped in Medicare Advantage Plans,” KFF Health News, January 5, 2024, https://kffhealthnews.org/news/article/medicare-advantage-medigap-enrollment-trap-switch-preexisting-conditions/.
- Cristina Boccuti et al., “Medigap Enrollment and Consumer Protections Vary Across States,” KFF, July 11, 2018, https://www.kff.org/medicare/issue-brief/medigap-enrollment-and-consumer-protections-vary-across-states/.
- Simon G. Talbot and Wendy Dean, “Physicians aren’t ‘burning out.’ They’re suffering from moral injury,” STAT News, July 16, 2018, https://www.statnews.com/2018/07/26/physicians-not-burning-out-they-are-suffering-moral-injury/.
- American Medical Association, “2022 prior authorization physician survey.”
- Ibid.
- Ibid.
- Medical Group Management Association, “Spotlight: Prior Authorization in Medicare Advantage,” May 2023, https://www.mgma.com/getkaiasset/fa2103f5-a2f6-47a1-b467-4748b5007c7e/05.03.2023_PA-in-MA_FINAL.pdf, 2.
- Ibid.
- Ibid., 5.
- Ibid.
- American Medical Association, “2022 prior authorization physician survey.”
- Hannah T. Neprash, et al., “Association of Primary Care Visit Length With Potentially Inappropriate Prescribing,” JAMA Health Forum, March 10, 2023, https://jamanetwork.com/journals/jama-health-forum/fullarticle/2802144#:~:text=The%20median%20physician%20in%20the,or%20less%20with%20their%20patients.
- Medical Group Management Association, “Annual Regulatory Burden Report,” November 2023, https://www.mgma.com/getkaiasset/423e0368-b834-467c-a6c3-53f4d759a490/2023%20MGMA%20Regulatory%20Burden%20Report%20FINAL.pdf, 5.
- Reed Abelson and Margot Sanger-Katz, “‘The Cash Monster Was Insatiable’: How Insurers Exploited Medicare for Billions,” New York Times, October 8, 2022, https://www.nytimes.com/2022/10/08/upshot/medicare-advantage-fraud-allegations.html.
- Physicians Advocacy Institute, “Physician Employment and Acquisitions of Physician Practices 2019-2021 Specialties Edition,” June 2022, https://www.physiciansadvocacyinstitute.org/Portals/0/assets/docs/PAI-Research/Physician%20Practice%20Trends%20Specialty%20Report%202019-2022.pdf?ver=MWjYUAcARbuGP9uxcgQkPw%3d%3d, 5.
- Richard M. Sheffler et al., “Monetizing Medicine: Private Equity and Competition in Physician Practice Markets,” American Antitrust Institute, July 10, 2023, https://www.antitrustinstitute.org/wp-content/uploads/2023/07/AAI-UCB-EG_Private-Equity-I-Physician-Practice-Report_FINAL.pdf, 4.
- Reed Abelson, “Corporate Giants Buy Up Primary Care Practices at Rapid Pace,” New York Times, May 12, 2023, https://www.nytimes.com/2023/05/08/health/primary-care-doctors-consolidation.html.
- Reed Abelson and Margot Sanger-Katz, “The Cash Monster was Insatiable.”
- Phil Galewitz, “Medicare Advantage plans shift their financial risk to doctors,” Modern Healthcare, October 8, 2018, https://www.modernhealthcare.com/article/20181008/NEWS/181009920/medicare-advantage-plans-shift-their-financial-risk-to-doctors.
Recommended Citation
Physicians for a National Health Program, “Taking Advantage: How Corporate Health Insurers Harm America’s Seniors,” May 23, 2024, https://pnhp.org/harmsreport.
Acknowledgements
Physicians for a National Health Program (PNHP) is grateful to the following individuals and organizations for their feedback and support. Without them, this report would not be possible:
- ASO Communications
- Diane Archer, Just Care USA
- Gretchen Jacobson, The Commonwealth Fund
- James G. Kahn, M.D., M.P.H.,University of California, San Francisco
- Eagan Kemp, Public Citizen
- David Lipschutz, Center for Medicare Advocacy
- Dhyan Wolf, Video Editor
We also wish to thank the dozens of patients, family members, physicians, allied health professionals, and Medicare supporters who shared their stories with us. Interview excerpts that appear in this report have been edited for clarity.
The PNHP Policy Committee worked closely with Communications Specialist Gaurav Kalwani to author this report. The committee consists of: Donald Bourne, M.D./Ph.D. 2027; Stephen Kemble, M.D.; Mark Krasnoff, M.D.; Susan Rogers, M.D.; Kip Sullivan, J.D.; Kay Tillow; James Patrick Waters, MS4; and Ed Weisbart, M.D.
The post Taking Advantage appeared first on PNHP.
Document Removed 7 May 2024 6:43 AM (11 months ago)
This document has been removed from public access for one of the following reasons:
- Privacy concerns
- Outdated content
- Incorrect content
- No longer available
If you require information from this document, please contact us to request access.
The post Document Removed appeared first on PNHP.
2023 Annual Meeting Materials 8 Nov 2023 6:53 PM (last year)
PNHP’s 2023 Annual Meeting in Atlanta drew physicians, students, and health justice activists from across the country for a weekend of learning, organizing, and direct action. Please see below to access a selection of archival recordings, slideshows, and handouts from the meeting. To view photos from the meeting, visit our Flickr page.
During the conference, we encouraged attendees to post to social media using the hashtag #PNHP2023. Click here to read member tweets, and be sure to follow PNHP on Twitter and Facebook so you can continue sharing single-payer content in the future.
Leadership Training (Nov. 10)
Agenda & schedule for the Leadership Training
Single Payer 101, presented by Diljeet Singh, MD, DrPH, Vice President, Physicians for a National Health Program (download slideshow here)
Welcome Message, presented by Philip Verhoef, MD, PhD, President, Physicians for a National Health Program
Transform your chapter’s people power into effective action, presented by Toby Terwilliger, MD, C0-Chair, PNHP Georgia Steering Committee; George Bohmfalk, MD, Chair, Health Care Justice – North Carolina; and Morgan Moore, Executive Director, Physicians for a National Health Program, NY Metro Chapter, (download slideshow here)
Narrative change and building relationships with elected officials, presented by Rebecca Cerese, Health Engagement Coordinator, Health Advocacy Project, North Carolina Justice Center; and Max Brockwell, Political Advocacy Co-Chair, Students for a National Health Program, (download slideshow here)
Introduction to direct action: agitate, educate, organize!, presented by Ksenia Varlyguina, MPH
Rooted in radical change: organizing, advocacy, mobilizing, presented by Andy Hyatt, MD, Board Adviser, Physicians for a National Health Program; and Richard Bruno, MD, MPH, Board Adviser, Physicians for a National Health Program
Building strong leaders and powerful SNaHP chapters, presented by James Moore, Media Co-Chair, Students for a National Health Program; and Yosha Singh, Executive Board Member, Students for a National Health Program, (download slideshow here)
Closing, debrief, and evaluation, presented by Lori Clark, National Organizer, Physicians for a National Health Program; and Ksenia Varlyguina, MPH
Lessons from house staff union organizing: Overcoming fear and building power, presented by Andy Hyatt, MD, Board Adviser, Physicians for a National Health Program (download slideshow here)
Annual Meeting (Nov. 11)
Agenda & schedule for the Annual Meeting
SNaHP Welcome: Building the single payer movement, presented by Ryan Parnell, Executive Board Member, Students for a National Health Program; Constance Fontanet, Infrastructure Co-Chair, Students for a National Health Program
Health Policy Update, presented by Adam Gaffney, MD, MPH, Past President, Physicians for a National Health Program; with James Waters, Executive Board Member, Students for a National Health Program, on Medicare Advantage, (Dr. Gaffney slideshow—with alternate visuals by Dr. Ed Weisbart—here; James Waters slideshow here)
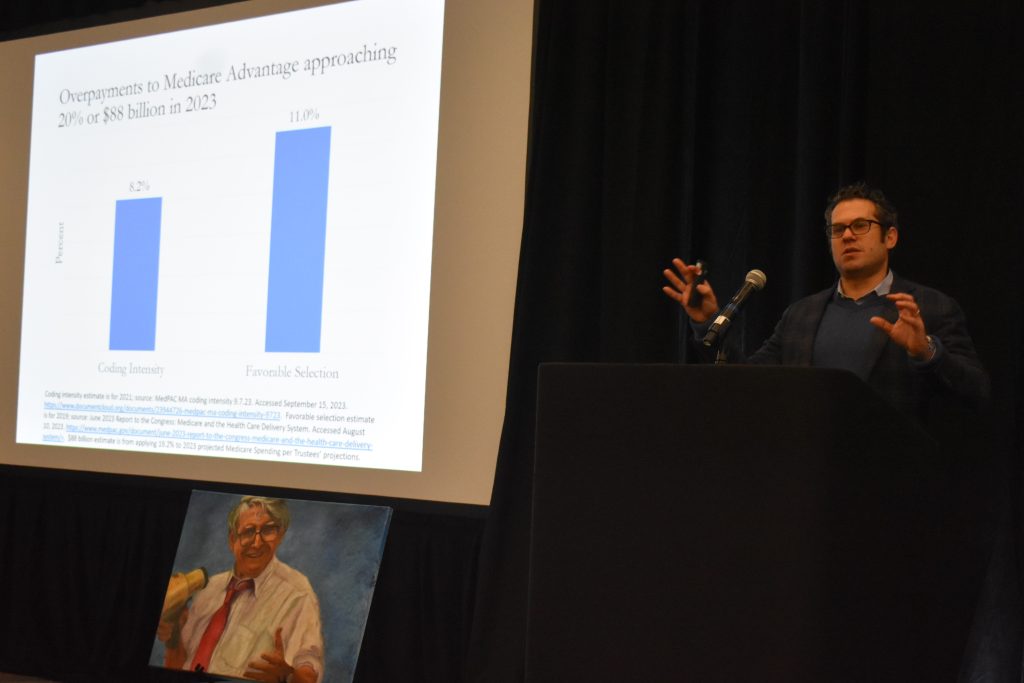
Messaging Medicare (dis)Advantage, by Jay Marcellus, Director of Narrative, ASO Communications, with an introduction by Ed Weisbart, MD, Board Secretary, Physicians for a National Health Program, (download Medicare Advantage messaging report here; access ASO Communications messaging guides here)
PNHP’s MA Campaign, presented by Jack Bernard, former Director of Health Planning for the State of Georgia
Building Progressive Power: Lessons from Georgia, discussion featuring Keron Blair, Chief of Field and Organizing, New Georgia Project; and Sanjeev Sriram, MD, MPH, National Board Member, Physicians for a National Health Program
SNaHP Plenary: SNaHP’s Moment to Move the Movement Forward, panel featuring Sanjeev Sriram, MD, MPH, National Board Member, Physicians for a National Health Program; Alankrita Olson, MD, National Board Member, Physicians for a National Health Program; and Richard Bruno, MD, MPH, Board Adviser, Physicians for a National Health Program; moderated by Robertha Barnes, Executive Board Member, Students for a National Health Program
Opportunities for federal action, presented by Alex Lawson, MPP, Executive Director, Social Security Works; and Amirah Sequeira, MPhil, Legislative Director, National Nurses United (learn more about the Medicare for All Act of 2023 here)
The “advantage” of stealth advocacy, presented by George Bohmfalk, MD, Chair, Health Care Justice – North Carolina; Corinne Frugoni, MD, Co-Chair, Humboldt Health Care for All/PNHP; Patty Harvey, Co-Chair, Humboldt Health Care for All/PNHP; and Ed Weisbart, MD, Board Secretary, Physicians for a National Health Program
Moral injury: What is it? How to talk about it and what the hell does it have to do with PNHP?, presented by Carol Paris, MD, National Board Member, Physicians for a National Health Program; Diljeet Singh, MD, DrPH, Vice President, Physicians for a National Health Program; and Janine Petito, MD, (download handout here)
Lessons from the labor movement, presented by Rose Roach, National Coordinator, Labor Campaign for Single Payer; and Rita Valenti, RN, Board Member, Healthcare-NOW!
Building a national movement through state and local organizing, presented by Mallika Sabharwal, MD, formerly active with Kentuckians for Single Payer Health Care; Ashley Duhon, MD, Board Adviser, Physicians for a National Health Program; Hugh Foy, MD, National Board Member, Physicians for a National Health Program; and Henk Goorhuis, MD, former Board Chair, Maine AllCare; moderated by Oliver Fein, MD, Chair, Executive Committee, Physicians for a National Health Program, NY Metro Chapter
Building your chapter’s power through game changing resolution campaigns, presented by Max Brockwell, Political Advocacy Co-Chair, Students for a National Health Program; and Joey Ballard, (download slideshow here)
The intersection of reproductive justice and single payer: The work continues, presented by Diljeet Singh, MD, DrPH, Vice President, Physicians for a National Health Program; Martha Livingston, PhD, Vice-Chair, Board of Directors, Physicians for a National Health Program, NY Metro Chapter; Michael Massey, Executive Board Member, Students for a National Health Program; Amir Jones; and Ashley Duhon, MD, Board Adviser, Physicians for a National Health Program, (download slideshow here)
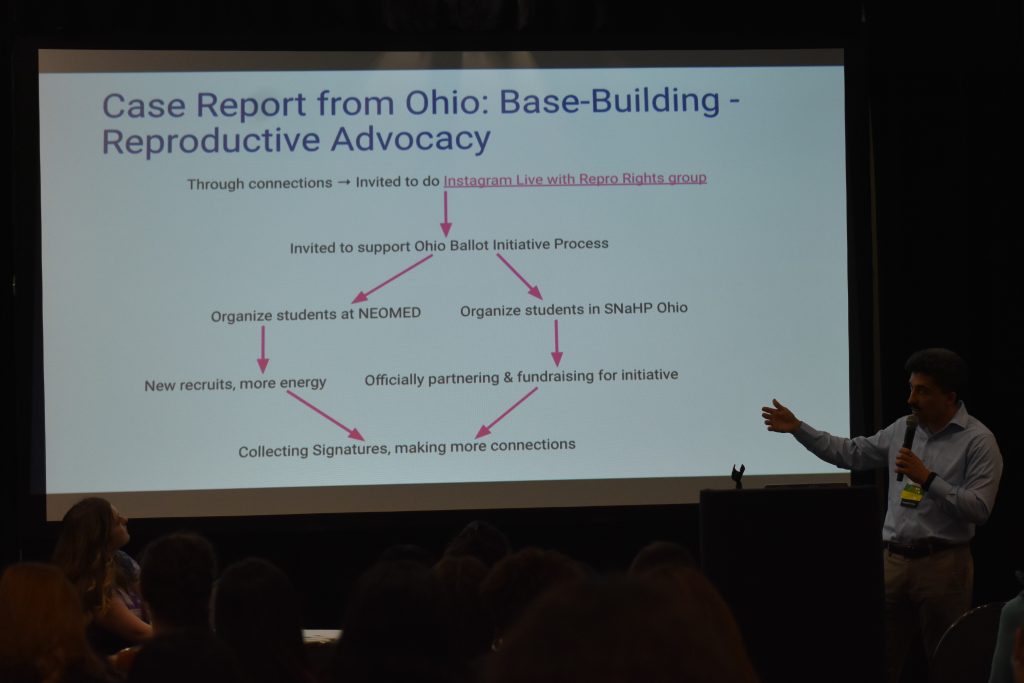
Addressing racist blindspots in our movement, presented by Sanjeev Sriram, MD, MPH, National Board Member, Physicians for a National Health Program; Robertha Barnes, Executive Board Member, Students for a National Health Program, (download slideshow here)
How Medicare for All can alleviate mass incarceration, presented by Mark Spencer, MD, (download slideshow here)
Problems of commodification in health care, presented by Martin Shapiro, MD, PhD, MPH; and Erin Fuse Brown, JD, MPH, (Dr. Shapiro slideshow here; Erin Fuse Brown slideshow here)
Keynote address: Confronting Racism Denial: Naming Racism and Moving to Action, by Camara P. Jones, MD, MPH, PhD, Past President, American Public Health Association, with an introduction by Robertha Barnes, Executive Board Member, Students for a National Health Program, (download slideshow here)
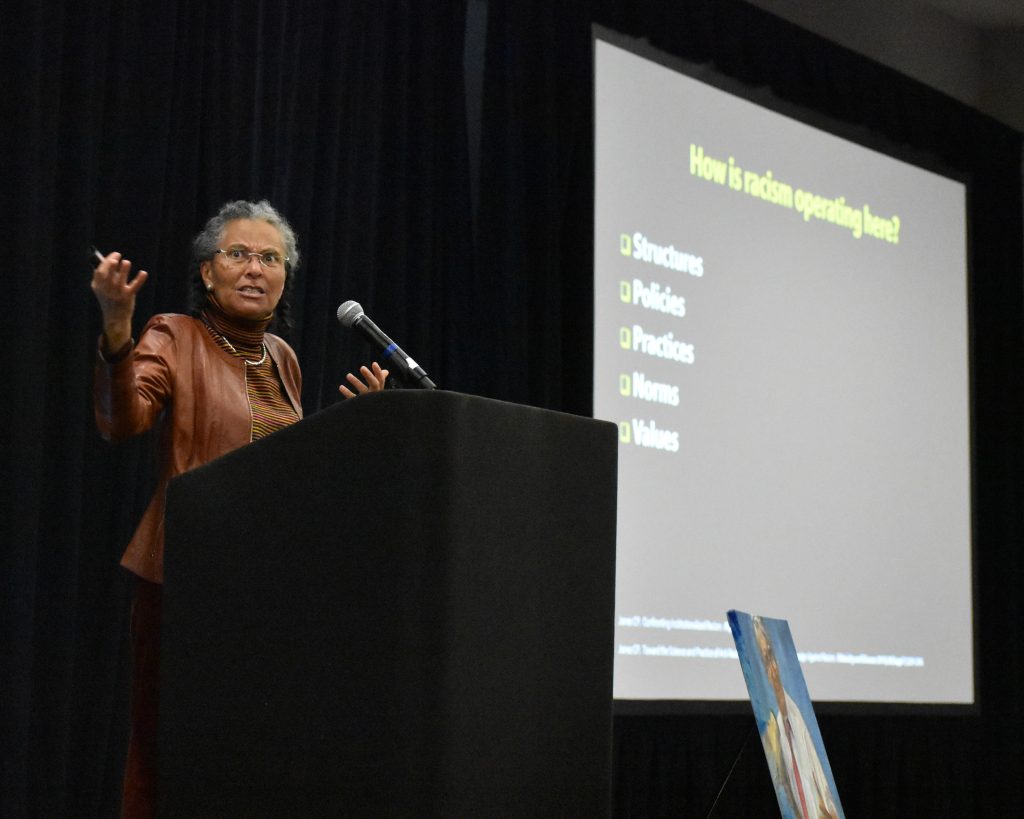
35th Anniversary Dinner
PNHP celebrated 35 years since our incorporation with a special anniversary dinner that included tributes to our allies, past presidents, student leaders, and co-founders.
- Program booklet (access PDF version here)
- Photos from our history (play slideshow here)
- 35th anniversary program (access slideshow here)
Health Activist Awards
Dr. Quentin Young Health Activist Award, presented to George Bohmfalk, MD, Chair, Health Care Justice – North Carolina by Diljeet Singh, MD, DrPH, Vice President, Physicians for a National Health Program
Dr. Quentin Young Health Activist Award, presented to Diljeet Singh, MD, DrPH, Vice President, Physicians for a National Health Program by Ashley Duhon, M.D., Board Adviser, Physicians for a National Health Program
Nicholas Skala Student Activist Award, presented to Donald Bourne, Executive Board Member, Students for a National Health Program by Ashley Duhon, M.D., Board Adviser, Physicians for a National Health Program

SNaHP Summit (Nov. 12)
Agenda & schedule for the SNaHP Summit
When you don’t think you can: An honest conversation about obstacles to advocacy, discussion featuring Philip Verhoef, MD, MPH, President, Physicians for a National Health Program; Claudia Fegan, MD, National Coordinator, Physicians for a National Health Program; Alankrita Olson, MD, National Board Member, Physicians for a National Health Program; and Ksenia Varlyguina, MPH; moderated by Emily Huff, Education Co-Chair, Students for a National Health Program
How to talk about single payer so people will listen, and listen so people will talk, presented by Emily Huff, Education Co-Chair, Students for a National Health Program; Cortez Johnson, Infrastructure Co-Chair, Students for a National Health Program; and Ed Weisbart, MD, Board Secretary, Physicians for a National Health Program (download slideshow here)
Building relationships and holding our elected officials accountable, presented by Edward Si, Executive Board Member, Students for a National Health Program; Ben Williams; and Carol Paris, MD, National Board Member, Physicians for a National Health Program, (download handout here)
Building your career in SNaHP and PNHP – Telling your health care advocacy story, by Isabella Pavkov, Infrastructure Co-Chair, Students for a National Health Program; and Michael Massey, Executive Board Member, Students for a National Health Program, (download slideshow here)
Stop Cop City: Intersections with health care and lessons learned, by Hamdi Abdi; Ruby Rousseau (download slideshow here)
Closing session, presented by Ryan Parnell, Executive Board Member, Students for a National Health Program; Constance Fontanet, Infrastructure Co-Chair, Students for a National Health Program
Public Action (Nov. 12)
PNHP members from across the country joined PNHP Georgia and local health justice activists for a march and rally demanding full Medicaid expansion in Georgia … and for the city to reclaim the recently closed Atlanta Medical Center and recommit to using it as a health resource for the community.

March starting at Martin Luther King Jr. National Park
Rally at the Atlanta Medical Center
This public action attracted media attention from the Atlanta Journal-Constitution (article here; medical student op-ed here). Less than one week later, it was reported that Georgia House Republicans were seriously considering full Medicaid expansion.
The post 2023 Annual Meeting Materials appeared first on PNHP.
Grand Rounds Speaker Resources 3 Nov 2023 2:43 PM (last year)
For 35 years, PNHP has been a trusted source of data and policy proposals, shedding light on our broken health care system and the promise of Medicare for All. Members of PNHP’s Grand Rounds speakers’ bureau have a unique opportunity to educate fellow health care providers about Medicare for All and recruit more like-minded physicians to our movement.
Below you will find sample slide sets in the consistent PNHP style, and additional resources to help you prepare for your next speaking event and encourage your audience to get involved.
Be sure to tell us about your speaking engagements by filling out THIS FORM. If you have questions, please contact National Organizer Rebecca Delay at rebecca@pnhp.org.
Sample Slide Sets
Featured presentations
- Medicare for All 101
- Health inequities and MFA
- Reproductive health and MFA
- Maternal mortality and MFA
- Mental health and MFA
Promoting PNHP to your audience
- Learn more about PNHP slide—add this to the end of your talks!
- Join PNHP slide—for audiences that are ready to become members today!
- Sign-up sheet (print PDF)
- Sign-up form (online version)
Add-ons
- Four key slides for presentations on Medicare for All (short)
- What is PNHP? (short)
- Why do Physicians want MFA? (short)
- How insurers harm seniors in Medicare Advantage (short)
Resources for Grand Rounds Speakers
- Tips for PNHP Grand Rounds Speakers (Google Doc)
- Tips for PNHP Grand Rounds Speakers (PDF)
- Health Policy Update from the 2023 PNHP Annual Meeting (PowerPoint)
- Recruiting Members through Presentations (Zoom training session; email admin@pnhp.org for the password to access the recording)
Recording of Grand Rounds Speakers Training
The post Grand Rounds Speaker Resources appeared first on PNHP.
PNHP Newsletter: Fall 2023 26 Oct 2023 1:34 PM (last year)
Table of contents
Click the links below to jump to different sections of the newsletter. To view a PDF version of the shorter print edition of the newsletter, click HERE.
If you wish to support PNHP’s outreach and education efforts with a financial contribution, click HERE.
If you have feedback about the newsletter, email info@pnhp.org.
PNHP News and Tools for Advocates
- PNHP Holds Messaging Training on Medicare Advantage
- Massachusetts Medical Society Passes Single-Payer Resolution
- PNHP Joins Be A Hero at DC Rally Against Corporate Profiteering in Medicare
- Meet Rebecca, Our New National Organizer
Come to Atlanta for PNHP’s Annual Meeting
Research Roundup
- Data Update: Health care crisis by the numbers
- Studies and analysis of interest to single-payer advocates
PNHP Chapter Reports
SNaHP Chapter Reports
- Florida State University
- Penn State
- University of Buffalo
- University of Minnesota-Twin Cities
- University of Missouri-Columbia
35th Anniversary House Parties
PNHP in the News
PNHP News and Tools for Advocates
PNHP Holds Messaging Training on Medicare Advantage
On August 24th, PNHP hosted a training for members and activists on how to talk about Medicare Advantage (MA) to different audiences. Drs. Ed Weisbart and Susan Rogers, as well as PNHP staff Dixon Galvez-Searle and Gaurav Kalwani, each gave an overview on the best tactics to use when speaking to physicians, members of the public, and policymakers about MA.
Below are some of the most important elements to consider in your own activism. These tips will be especially helpful when you are attempting to get people to fill out our beneficiary and physician surveys, sign our MA petition, and join PNHP.
For Physicians
- Connect with personal and patient stories: Regardless of their level of policy knowledge, physicians will resonate most with your own stories of how MA has brought harm to your patients or others.
- Focus on professional autonomy: Emphasize the ways in which MA prevents physicians from doing their jobs, by making them deal with prior authorization, claim denials, and other headaches. Make sure you name specific insurance companies as the culprit here.
For the General Public
- Qualify the term “Medicare Advantage”: While it’s best to be clear when using the term Medicare Advantage and avoid potentially turning someone off with terms like “Medicare Disadvantage,” you can emphasize the problems with the program by calling it something like “corporated-controlled Medicare Advantage” or “so-called Medicare Advantage.”
- Focus on “reclaiming” Medicare: Remind people that Medicare is their program, paid for by their tax dollars, which are currently being funneled into big insurance companies while undermining our beloved public insurance programs.
For Policymakers
- MA is radically changing Medicare: Remind them that Medicare was created to be a social insurance program, and that letting insurers take it over is a fundamental change to that model. Insurer “innovations” like narrow networks and prior authorization are contrary to the spirit of the program, lead to worse care outcomes, and have no place in Medicare.
- MA redirects public dollars to private hands: MA costs more than TM, and that money is going directly from taxpayers into corporate profits. This money was supposed to be spent on patient care, and it should be.
For Everyone
- Lead with shared values, not problems: You’ll have more success connecting with people by opening with easily agreeable statements. Data supports focus on family, community, fairness, and freedom, so use openings like: “Do you have a minute to talk about making sure seniors in our community get the best possible care?”
- Don’t shield the culprits from view: Insurance companies are not well-liked by anybody in this country, so it’s important to make them the face of Medicare Advantage, rather than the government. Make sure to specify the companies doing harm here, and show that they are the ones raiding the Medicare trust fund. Avoid using statements that imply the government is “broken”, which could make private alternatives seem more attractive.
- Focus on tangible patient harms: Have stories and data ready to go that show why narrow networks, surprise bills, and care delays/denials are harmful and even fatal to patients. Explain how traditional Medicare does not have these problems, and why private insurance always will.
- Inspire hope: Don’t exclusively go negative, because we want people to believe that things can change. Talk about the improvements we want to see in Medicare, and the future we’re fighting for.
Find more materials on Medicare Advantage in our latest Kitchen Table Campaign toolkit, and at ProtectMedicare.net.
Massachusetts Medical Society Passes Single-Payer Resolution
Following many months of intense and dedicated organizing by PNHP members and allies in the state, the Massachusetts Medical Society (MMS) House of Delegates passed a resolution stating:
“That the MMS supports and will advocate for universal access to equitable, comprehensive, affordable, high-quality, administratively streamlined health care through a national health program, as well as through legislation at the state level, and will continue to explore and evaluate payment structures that may be able to achieve these goals.”
This exciting development in Massachusetts offers inspiration and several useful lessons for members to apply in their own efforts to pass single-payer resolutions in various regional and specialty-based medical societies.
Dr. C. Frazer Shipman, a member of PNHP for 30 years, helped lead this campaign from the beginning. The effort began at the district-level, with a resolution based on one of PNHP’s sample resolutions receiving positive feedback in the Franklin District Medical Society, and from there making its way to the full state House of Delegates in 2022. Over the next year, the resolution team recruited many PNHP members who were also part of the MMS to testify in support of the resolution. Because of these efforts, testimonies were 3-to-1 in favor of single payer.
“I used PNHP data and their sample resolution to work with members of my local district,” said Dr. Shipman. “Many Mass physicians and Medicare for All advocates worked hard to pass the wording quoted above, including the Berkshire and Hampshire Districts, PNHP National, the Boston PNHP Chapter, and Mass-Care.”
By working together with like-minded allies, understanding the environment of their medical society, and planning an extensive campaign of recruitment and engagement, these physicians and advocates were able to push Massachusetts health care in a more progressive direction.
If you would like to do the same in your local medical society, please reach out to our national organizer, Lori Clark, at lori@pnhp.org to discuss beginning your own resolution campaign.
PNHP Joins Be A Hero at DC Rally Against Corporate Profiteering in Medicare

On July 25th, PNHP joined with Be a Hero and other organizational allies as well as members of Congress like Senator Elizabeth Warren (D-MA), Rep. Mark Pocan (D-WI), and Rep. Barbara Lee (D-CA) to rally against corporate raiding of taxpayer dollars through the Medicare Advantage program.
Members of Congress and advocates alike spoke about the myriad issues with Medicare Advantage, told personal stories of loved ones who were harmed by the greed of the insurance industry, and demanded a true solution to the health care woes of this country that would provide coverage to each and every person.
Introducing Rep. Lee, PNHP’s own Dr. Steve Auerbach stated the problem succinctly. “Denials and delays and narrow networks are killing Americans every day,” he said. “The leeches of private insurance are sucking out taxpayer dollars that should be going to patient care. Medicare Disadvantage is bad for patients, doctors, and hospitals.”
Several members of Congress pointed to issues in prior authorization, upcoding, and other abuses that give away money to corporate insurers while leading to worse care for seniors and people with disabilities.
“It is time to crack down on these abuses,” said Senator Warren. “Instead of giving away extra money to private insurance companies, we can strengthen traditional Medicare.”
The rally was followed by a day of lobbying, wherein advocates visited various Congressional offices to speak with their elected officials on the need to crack down on the corrupt and corporate-controlled Medicare Advantage program.
Meet Rebecca, Our New National Organizer

Previous Experience: I am a recent Master’s in Public Policy graduate with a certificate in health policy. The scope of my experience ranges from Congressional intern to lobbying with Planned Parenthood and publishing research in The Contraception Journal.
What drew you to PNHP? Throughout my career, I have been trying to find the bridge between my interests in health and medicine, with the world of politics. PNHP provided me the outlet to use my health policy background to pursue my personal activism goals.
What are you looking forward to working on over the next 12 months? I am excited to bring a rejuvenated enthusiasm to the PNHP team and network. I also look forward to creating partnerships within the single-payer movement with other social justice organizations.
What’s a fun fact about yourself? I am a dedicated sports fan, originally from Oakland, CA. Go Raiders!
Come to Atlanta for PNHP’s Annual Meeting and 35th Anniversary celebration

PNHP’s 2023 Annual Meeting and Leadership Training, along with the 2023 SNaHP Summit, will be held Nov. 10-12 in Atlanta. We will celebrate 35 years since PNHP’s incorporation, strategize for the path to achieving Medicare for All, and hear from our keynote speaker, Dr. Camara Jones.
Camara P. Jones, M.D., M.P.H., Ph.D., is a family physician, epidemiologist, and past president of the American Public Health Association whose work focuses on naming, measuring, and addressing the impacts of racism on the health and wellbeing of the United States and the world.
When planning your travel, don’t forget to join us for PNHP’s 35th Anniversary celebration dinner on Saturday, Nov. 11, and stay for a public action on Sunday, Nov. 12. More event details (including hotel booking information and meeting registration) can be found at pnhp.org/meeting.
You can send a student to the 2023 SNaHP Summit, being held in Atlanta in conjunction with PNHP’s Annual Meeting, by making a gift to the Nick Skala Student Activist Fund. Use the card enclosed with this newsletter or go to pnhp.org/SkalaFund to support the future of our movement.
Research Roundup
Data Update: Health Care Crisis by the Numbers
Barriers to Care
At least 1.7 million Americans rely on health sharing plans: Data from 16 sharing plans provided the first national count of the number of Americans relying on these schemes, which arrange for people to pay one another’s medical bills. At least 11 of the plans operated in or advertised in all 50 states; these plans are usually organized around people with common religious beliefs. Because sharing plans are not held to the same consumer protections and regulations as insurance plans, costs can easily spiral out of control. Markian Hawryluk, “At Least 1.7M Americans Use Health Sharing Arrangements, Despite Lack of Protections,” KFF Health News, 6/14/23.
Majority of insured adults experience problem using health coverage: 58% say they have experienced a problem using their insurance in the past 12 months–these include denied claims, network issues, and pre-authorization issues. Adults in fair or poor health as opposed to good health were more likely to experience problems, with 67% of these adults reporting an issue. Among the 58% who had problems, 17% were unable to receive recommended care as a result. 15% experienced a decline in their health, and 28% said they paid more than they expected for care. Pollitz et al., “KFF Survey of Consumer Experiences with Health Insurance,” KFF, 6/15/23.
Data on denials is shrouded in mystery: There is a serious lack of transparency around data on insurance claim denials. Limited government data suggests insurers deny between 10% and 20% of claims, but these are only aggregated numbers and do not explore differences in types of care or insurance. 85% of people with insurance say they want regulators to compel insurers to disclose how often they deny claims. Robin Fields, “How Often Do Health Insurers Say No to Patients? No One Knows,” ProPublica, 6/28/23.
Hospital consolidation leads to inpatient pediatric service closures: A study in JAMA Pediatrics found that inpatient pediatric services had decreased across the study period, going from being offered at 41.5% of 4,876 hospitals in 2011 to 32.6% of 4,551 hospitals in 2020. Of 1,088 hospitals further studied, 235 joined a larger health system during the study period. Joining a larger health system was significantly associated with a loss of inpatient pediatric services within five years. Dave Muoio, “Hospital consolidation followed by inpatient pediatric service closures, study finds,” Fierce Healthcare, 6/6/23.
Healthcare costs projected to grow 7% in 2024: Factors accounting for this increase include providers dealing with higher expenses and seeking rate increases during contract negotiations with insurers. The projection, made by consultants at PricewaterhouseCoopers, tops previous estimates in 2022 and 2023, which were 5.5% and 6%, respectively. To create these estimates, the consultancy spoke with actuaries who work with insurers covering 100 million employer-sponsored members and 10 million Affordable Care Act members to forecast healthcare inflation. Results were weighted by each health plan’s size. Alex Kacik, “Healthcare costs to grow 7% next year: PwC,” Modern Healthcare, 6/29/23.
Patients with Parkinson’s disease face barriers seeing a neurologist: An estimated 90% of people living with Parkinson’s disease (PD) in the U.S. are covered by Medicare. PD beneficiaries number 685,116, or 1.2% of the total Medicare population. Compared to the overall Medicare population, 56.3% are male (vs 45.6%), 77.9% over age 70 (vs 57.1%), 14.7% people of color (vs 20.7%), and 16.0% are rural residents (vs 17.5%). 40% of PD beneficiaries did not see a neurologist at all during the calendar year, and only 9.1% visited a movement disorder specialist. Few beneficiaries diagnosed with PD use recommended services such as physical, occupational, or speech therapy. People of color and rural residents were least likely to access a neurologist or therapy services. Despite 52.9% of beneficiaries being diagnosed with depression, only 1.8% had a clinical psychology visit. Pearson et al., “Care access and utilization among Medicare beneficiaries living with Parkinson’s disease,” NPJ Parkinson’s Disease, 7/10/23.
Youth face issues accessing opioid addiction medication: From 2015 to 2020, the proportion of buprenorphine prescriptions dispensed for youths age 12-19 decreased for commercial insurance from 29.8% to 22.9%, for self-pay from 13.2% to 7.6%, and for assistance from 18.2% to 8.9%. While total prescriptions dispensed decreased 17.5%, the proportion of prescriptions paid by Medicaid, the payer with the greatest share of prescriptions in 2020, increased from 27.1% to 44.3%. In the South, prescriptions had higher out of pocket costs, a higher proportion were paid by self-pay and assistance, and a lower proportion were paid by Medicaid. Prescriptions in rural counties followed similar patterns to the South. Terranella et al., “Out-of-Pocket Costs and Payer Types for Buprenorphine Among US Youth Aged 12 to 19 Years,” JAMA Pediatrics, 8/7/23.
Price of elder care continues to increase: Fueled by increases in the elderly population, the price of nursing home care increased by an average of 2.4% each year between 2012 and 2019, for a cumulative increase of 20.7%. In 2021, the median cost to stay in a private room in a nursing home in the U.S. is $9,034 per month. The median cost to stay in a semi-private room in a nursing home was $7,908 a month, and the median cost to stay in an assisted living facility was $4,500 per month. Alejandra O’Connell-Domenech, “Price of elder care soars as demand increases, baby boomers age,” The Hill, 8/13/23.
Medicare & Medicaid Issues
Medicaid disenrollments continue: As of August 24, at least 5.4 million Americans have lost their Medicaid coverage. Disenrollment rates vary from 72% in Texas to 8% in Wyoming. Across all states, 74% of people have lost coverage for procedural reasons rather than changing eligibility. In the 15 states reporting age breakouts, more than 40% of disenrollments were of children. KFF, “Medicaid Enrollment and Unwinding Tracker,” 8/24/23.
Crowdfunding is only hope for many diabetes patients: A study examining 313 crowdfunding campaigns found that the median goal for campaigns was $10,000, and only 14% of campaigns reached their goal, though with a median of $2,600 raised. 27% of people said they had insurance, but nearly all said their out of pocket costs were too high or coverage was too sparse. 6% requested money specifically for insulin, 10% requested money for insulin pumps, and 6% requested money for a continuous glucose monitor. Kristen Monaco, “When Insurance Doesn’t Cut It, Diabetes Patients, Turn To Crowdfunding,” MedPage Today, 6/7/23.
Medicare Advantage Payments higher than previously estimated: MedPAC has estimated annual overpayments in Medicare Advantage to be about 6% of $27 billion. A new study estimates that, because of the impact of “favorable selection,” this amount is actually closer to more than 20% or $75 billion annually. Adriel Bettelheim, “Medicare Advantage overpayments higher than estimated: study,” Axios, 6/14/23.
Medicare Advantage quality bonus program has questionable benefits: Combined, United Healthcare and Humana received $4.7 billion in bonuses for their MA plans last year. Issues in star rating calculation, difficulty in measuring quality, and rating inflation contribute to a system where payments do not reflect actual quality of care. In 2014, the average star rating across Medicare Advantage contracts was 3.86, compared with 4.15 in 2023. Mari Devereaux, “Medicare Advantage quality bonus program needs reform: Urban Institute,” Modern Healthcare, 7/6/23.
Medicare Advantage insurer pays largest fraud settlement in Maine state history: Martin’s Point Health Care Inc. will pay almost $22.5 million to resolve allegations of submitting inaccurate codes for MA enrollees to increase Medicare payments. The company was accused of submitting inaccurate diagnosis codes for enrollees in Maine and New Hampshire between 2016 and 2019. The allegations against the provider originated from a whistleblower complaint; the whistleblower will receive a portion of the settlement, around $3.8 million. AP, “Health care provider to pay largest Medicare fraud settlement in Maine history,” 7/31/23.
CMS sets higher payment hikes for hospitals: Inpatient hospitals will receive a higher rise in payments from CMS than initially proposed. Acute care hospitals in compliance with various guidelines will receive a 3.1% net increase in Medicare payments in fiscal 2024, an increase from the original hike of 2.8% proposed in April. CMS also set a 0.2% reimbursement increase for long-term care hospitals. Lauren Berryman, “CMS sets pay hikes for inpatient, long-term care hospitals,” Modern Healthcare, 8/1/23.
Georgia Medicaid work program off to slow start: Despite projections from the Georgia Department of Community Health that indicated up to 100,000 people could benefit from Georgia’s Medicaid work program, known as Pathways to Coverage, just 265 applications had been approved by August of this year. At the same time, Georgia has cut more than 170,000 adults and children from Medicaid as it continues its review of the 2.7 million Medicaid recipients in the state. Sudhin Thanawala, “Georgia Medicaid program with work requirement off to slow start even as thousands lose coverage,” AP, 8/19/23.
Pharma
Severe shortages in cancer drugs: A survey of cancer centers revealed that 93% of centers are experiencing a shortage of carboplatin, and 73% are experiencing a shortage of cisplatin. These medications are used to treat a wide variety of cancers, including lung, breast, prostate, and gynecologic cancers, as well as lymphomas and leukemias. Only 64% of centers reported being able to keep all patients on a carboplatin regimen without delays or claim denials. National Comprehensive Cancer Care Network, “NCCN Releases Statement Addressing Ongoing Chemotherapy Shortages; Shares Survey Results Finding More than 90% of Cancer Centers are Impacted,” 6/7/23.
Large drug distributor sued by tribe over opioid crisis: A lawsuit was filed by the Cherokee Nation on behalf of the entire 400,000-citizen tribe in Oklahoma state court, alleging negligence on the part of the distributor, Morris & Dickson. The suit states that between 2010 and 2014, the distributor shipped more than 3.7 million pills to just five pharmacies in counties populated by tribal members. More than 5,200 people died of drug overdoses in Oklahoma from 2014 to 2020. David Ovalle, “Opioid distributor, already facing license revocation, sued by tribe,” Washington Post, 6/8/23.
Drug and supply chain burdens plague health systems: Large health systems are seeing shortages of upwards of 600 products and 200-300 drugs a month. Providers are 2.5 times more likely to experience shortages on products in markets that have two or fewer manufacturers accounting for more than 80% of market share. Nearly half of respondents (48.6%) to a survey of health and supply chain officials said they had to cancel or reschedule cases or procedures at least quarterly in 2022 due to product shortages. Adriel Bettelheim, “Health systems plagued by spot shortages scramble for essentials,” Axios, 6/29/23.
$2.9 million gene therapy for severe hemophilia approved by FDA: Roctavian was approved for adult patients with severe cases of hemophilia A. Approval was based on a three-year study showing a 50% reduction in annual bleeding incidents among 134 patients who received the treatment. Traditional infusions for this condition cost about $800,000 annually for a typical patient. The maker estimates about 2,500 U.S. patients will be eligible to receive the therapy under the terms of the FDA’s approval. Last year, Hemgenix, a similar gene therapy for hemophilia B, was approved and became the most expensive drug of all time at $3.5 million. Matthew Perrone, “$2.9 million gene therapy for severe hemophilia is approved by FDA,” AP, 6/29/23.
Nevada reaches $1 billion in total opioid settlements: Nevada reached a $285 million settlement with Walgreens regarding the chain’s role in the opioid epidemic. Nevada’s total anticipated payments from opioid claims now amount to $1.1 billion. Most recently, the state reached a $193 million agreement with Teva Pharmaceuticals in June and a $152 million deal with CVS in May. AP, “Nevada secures $285M opioid settlement with Walgreens, bringing total settlements to $1 billion,” 7/5/23.
5 largest pharma firms earned $81.9 billion last year: The combined stock buybacks and dividends of the companies increased by $4.4 billion and $2.5 billion, respectively, from 2021 to 2022. Pfizer’s net income was over $31.4 billion during fiscal 2022, a 42.5% increase from 2021. Shareholders of Pfizer received more than $10.9 billion in stock dividends and buybacks. Last year, Merck’s net income was over $14.5 billion, and more than $7 billion was spent on shareholder dividends. Taylor Giorno, “Top 5 largest US pharma firms’ net earnings topped $81.9 billion last year: watchdog,” The Hill, 7/24/23.
Uninsured patients paying up to $330 for Eli Lilly’s insulin: Despite the company’s pledge to cut its list price for its insulin to $25 per vial, a survey of more than 300 pharmacies across all 50 states by Senator Elizabeth Warren’s office found that uninsured patients paid an average of $98 for the drug. A third of drug stores charged $164 or more for the company’s insulin, with the highest-priced pharmacy charging $330. Chain stores charged uninsured patients an average of $123 per vial, compared to $63 at independent pharmacies. Patrick Wingrove, “Uninsured US patients pay up to $330 for Eli Lilly’s $25 insulin, Senator Warren says,” Reuters, 7/13/23.
Health Inequities
Burden of obesity falls on marginalized groups: Non-Hispanic Black adults have the highest obesity rates of any racial group–four out of five Black women have obesity. Approximately 45.6% of Hispanic adults are living with obesity as well. The prevalence of obesity is six times higher in rural America compared to urban America, and poverty is strongly correlated with obesity. Despite this, coverage is limited, and less than 2% of those eligible for anti-obesity medications are prescribed them. Health Equity Coalition for Chronic Disease, “Advancing Equity: The Urgent Need to Confront Disparities in Obesity,” June 2023.
OBGYNs say effects of Dobbs decision overwhelmingly negative: 68% of 569 board-certified OBGYNs surveyed say the effects of the decision have made the management of pregnancy-related emergencies worse, while 64% say the ruling has worsened pregnancy-related mortality. 70% believe that the decision has widened racial and ethnic inequities in maternal health care. 61% of OBGYNs practicing in states where abortion is banned are worried about their own legal risk when making decisions on patient care. Kim Bellware and Emily Guskin, “Effects of Dobbs on maternal health care overwhelmingly negative, survey shows,” Washington Post, 6/21/23.
Black, rural, southern women most in need of maternal care assistance aren’t getting it: Not one site funded by a federal program created to improve rural maternity care is located in the Southeast, which has the largest concentration of predominantly Black rural communities. Among the initial 2019 grant awardees, the awardee in Texas reported that 91% of people it served were Hispanic. New Mexico’s awardee reported that 59% of recipients were Hispanic, and Missouri reported that 22% of beneficiaries were Black. In all cases, the majority were Medicaid enrollees. Sarah Jane Tribble, “Black, Rural Southern Women at Gravest Risk From Pregnancy Miss Out on Maternal Health Aid,” KFF Health News, 6/22/23.
Transgender individuals face higher suicide rates: A study of individuals in Denmark found that transgender individuals had a rate of suicide attempts 7.7 times higher than nontransgender individuals. The study also found that transgender individuals have a 3.5 times higher suicide mortality and a 1.9 times higher suicide-unrelated mortality Suicide attempt rates per 100,000 person–years were 498 for transgender individuals and 71 for nontransgender individuals. Erlangsen et al., “Transgender Identity and Suicide Attempts and Mortality in Denmark,” JAMA, 6/27/23.
State-level maternal mortality rates are higher for Black and Native individuals: In 2019, maternal mortality rates in most states were higher among American Indian and Alaska Native and Black populations than among Asian, Native Hawaiian, or Other Pacific Islander; Hispanic; and White populations. Between 1999 and 2019, observed median state mortality rates increased from 14 to 49.2 among the American Indian and Alaska Native population, 26.7 to 55.4 among the Black population, 9.6 to 20.9 among the Asian, Native Hawaiian, or Other Pacific Islander population, 9.6 to 19.1 among the Hispanic population, and 9.4 to 26.3 among the White population. In each year between 1999 and 2019, the Black population had the highest median state maternal mortality rate. Fleszar et al., “Trends in State-Level Maternal Mortality by Racial and Ethnic Group in the United States,” JAMA, 7/3/23.
Rural Americans struggle to afford health care: As compared with similarly high-income nations, rural Americans have a harder time affording medical care and are more likely to skip care because of costs. 22.8% of rural Americans have had serious problems paying or were unable to pay medical bills, compared to 8.9% of rural Australians and 6.5% of rural Canadians. Similarly, 36% of rural Americans skipped needed care due to costs, compared with 14.4% of rural Canadians and 11.3% of rural French. Munira Z. Gunja, “Rural Americans Struggle with Medical Bills and Health Care Affordability,” The Commonwealth Fund, 7/24/23.
Hispanic families kept out of Medicaid by poor administration: Reaching someone at Florida Medicaid’s call center took an average of two and a half hours for Spanish speakers, compared with 36 minutes for English speakers. The longest delay experienced for an English speaker in the study was just 50 minutes, far shorter than the average wait for Spanish speakers. Almost a third (30%) of all Spanish calls were disconnected before the caller reached a human being; by contrast, only 10% of English calls were dropped. UnidosUS, “At Florida’s Medicaid call center, long and discriminatory delays prevent eligible families from keeping their health care,” 8/17/23.
Profiteers in Health Care
California hospitals ask for bailout despite billions in profits: The California Hospital Association has requested a $1.5 billion bailout from the state government, despite the hospital industry taking in $9.2 billion in patient revenue in 2021. One of the country’s richest hospitals, Cedars-Sinai Health System in Los Angeles, received a $28 million grant from a charity that collects money from other hospitals, many of which serve California’s poorest residents. Samantha Young and Angela Hart, “California Hospitals Seek a Broad Bailout, but They Don’t All Need It,” KFF Health News, 5/5/23.
Class action lawsuit against Aetna and Optum proceeds: A judge for the U.S. District Court for the Western District of North Carolina certified the class-action lawsuit, which includes more than 87,700 people and nearly 2,000 health plans. The suit alleges that Aetna and Optum used misleading billing practices, developing “dummy code” that was intended to bury fees and pass off administrative fees as medical expenses. The initial plaintiff sued in 2015 after her cost for physical therapy doubled under an Aetna plan. Nona Tepper, “Aetna, Optum to face revived ‘dummy code’ lawsuit,” Modern Healthcare, 6/7/23.
Fraudsters trick poor and homeless people into signing up for unaffordable ACA plans: The federal agency overseeing the marketplace said that for the fiscal year ending September 30, 2022, the agency received more than 25,000 complaints from people saying that they had been enrolled in policies without their consent or that incorrect information was submitted for them by an agent or broker. CMS said it performed more than 700 license verifications because of these issues during the same period. Daniel Chang, “Fraudsters Are Duping Homeless People Into Signing Up for ACA Plans They Can’t Afford,” KFF Health News, 6/13/23.
Nonprofit hospitals collect public money while exacerbating debt: 41% of adults in the U.S. have some form of medical debt, and 73% of adults with past-due medical debt report owing at least some of that debt to hospitals. Nearly 60% of community hospitals in the country are privately operated nonprofits, and while these nonprofit hospitals received $28 billion in tax benefits in 2020, they only spent about $16 billion on free or reduced-price charity care. The median nonprofit hospital only spends 1.5% of hospital expenses on charity care. Brian Stauffer, “In Sheep’s Clothing: United States’ Poorly Regulated Nonprofit Hospitals Undermine Health Care Access,” Human Rights Watch, 6/15/23.
Physician-owned hospitals have lower costs: An analysis of around 1,100 non-physician owned hospitals and 150 physician-owned hospitals found that prices negotiated between hospitals and commercial insurers for eight common procedures were 33.7% lower at physician-owned hospitals compared with non-physician owned hospitals. This could potentially be due to the fact that physician-owned hospitals treat fewer Medicaid patients and provide less charity care, although these factors were controlled for in the study. Wang et al., “Comparison of Commercial Negotiated Price and Cash Price Between Physician-Owned Hospitals and Other Hospitals in the Same Hospital Referral Region,” JAMA Network Open, 6/23/23.
Private equity grows in anesthesiology and emergency medicine: From 2009 to 2019, physician groups owned by private equity or publicly traded companies grew from 3.2% and 8.6% of the national anesthesia and emergency medicine markets, respectively, to 18.8% and 22.0%. Over the same period, the five largest independent anesthesia practices and five of the six largest independent emergency medicine practices were acquired by private equity or publicly traded companies. Also during this period, the share of the population living in a highly concentrated anesthesia market increased from 16.8% to 34.4%. Adler et al., “Measuring private equity penetration and consolidation in emergency medicine and anesthesiology,” Health Affairs Scholar, July 2023.
Biden administration takes aim at facility fees: The Biden administration announced a plan to mandate transparency in facility fees, which are charged by hospitals when they provide services in an outpatient location. In 2022, a 15-minute doctor visit in a hospital-owned clinic cost Medicare $189, of which facility fees accounted for $121 of the charge. The same visit cost $92 in a freestanding doctor’s office. Between 2004 and 2021, facility fees in emergency departments rose by 531%. Annalisa Merelli, “New Biden initiative targets controversial hospital ‘facility fees’ that often surprise patients,” STAT News, 7/7/23.
Health CEOs made more than $4 billion last year: The CEOs of more than 300 publicly traded health care companies made a combined $4 billion in 2022. This number is actually an 11% decrease from the $4.5 billion CEOs made in 2021. The 10 highest-paid CEOs made a collective $1.4 billion. The average health CEO salary for 2022 was $13 million. The median bonus payment for these CEOs was around $700,000. Once again, the highest-paid CEO overall was Moderna’s Stéphane Bancel, who took in $398 million. Herman et al., “Health care CEOs hauled in $4 billion last year as inflation pinched workers, analysis shows,” STAT News, 8/17/23
Studies and analysis of interest to single-payer advocates
“Alleviating Medical Debt in the United States,” by Nishant Uppal, M.D., M.B.A.; Steffie Woolhandler, M.D., M.P.H.; and David U. Himmelstein, M.D., New England Journal of Medicine, 9/7/23. “The persistence of medical debt and low levels of charity care at nonprofit hospitals (despite the financial assistance mandate in the Affordable Care Act) indicate that more muscular policies are needed.”
“How Health Insurers and Brokers Are Marketing Medicare,” Jeannie Fuglesten Biniek; Alex Cottrill; Nolan Sroczynski; Meredith Freed; Tricia Neuman; Breeze Floyd; Laura Baum; and Erika Franklin Fowler, KFF, 9/15/23. “TV ads for Medicare Advantage often showed images of a government-issued Medicare card or urged viewers to call a ‘Medicare’ hotline other than the official 1-800-Medicare hotline. More than a quarter of all airings (27%) included a government-issued Medicare card or image that resembled it, including 28% of insurer-sponsored airings and 21% of airings sponsored by brokers and other third-party entities, a trend that CMS has flagged as potentially misleading to beneficiaries. Roughly 16% of airings featured a privately-run phone line described as a ‘Medicare’ hotline, most of which were sponsored by brokers and other third-party entities.”
“Medicare’s Affordability Problem: A Look at the Cost Burdens Faced by Older Enrollees,” by Faith Leonard; Gretchen Jacobson; Sara R. Collins; Arnav Shah; and Lauren A. Haynes, Commonwealth Fund, 9/19/23. “The likelihood of having problems paying medical bills or debt was significantly higher for older adults with Medicare Advantage than those with traditional Medicare. Differences in the percent with medical bill or debt problems were significant among those with income between 200 percent and 399 percent of FPL and not statistically significant for those with higher or lower incomes.”
“Our Payments, Their Profits: Quantifying Overpayments in the Medicare Advantage Program,” by Physicians for a National Health Program, October 2023. “By our estimate, and based on 2022 spending, Medicare Advantage overcharges taxpayers by a minimum of 22% or $88 billion per year, and potentially by up to 35% or $140 billion. By comparison, Part B premiums in 2022 totaled approximately $131 billion, and overall federal spending on Part D drug benefits cost approximately $126 billion. Either of these—or other crucial aspects of Medicare and Medicaid—could be funded entirely by eliminating overcharges in the Medicare Advantage program.”
“Tiny, Rural Hospitals Feel the Pinch as Medicare Advantage Plans Grow,” by Sarah Jane Tribble, KFF Health News, 10/23/23. “Medicare Advantage growth has had an outsize impact on the finances of small, rural hospitals that Medicare has designated as ‘critical access.’ Under the designation, government-administered Medicare pays extra to those hospitals to compensate for low patient volumes. Medicare Advantage plans, on the other hand, offer negotiated rates that hospital operators say often don’t match those of traditional Medicare.”
PNHP Chapter Reports
Georgia
In Georgia, members held a 35th anniversary social and fundraiser, attracting over 40 attendees and raising just over $2000. The chapter also hosted the Atlanta premiere of “American Hospitals,” as well as a Universal Health Care Symposium at Grady Memorial Hospital.
To get involved in Georgia, please contact Dr. Elizabeth McCord at eomccord@gmail.com.
New Hampshire
In New Hampshire, members of Granite State PNHP hosted two public screenings of the film “American Hospitals,” and held post-film panel and discussion sessions. The chapter is also currently planning a campaign to have the New Hampshire Medical Society pass a resolution endorsing a “Simplified Public Payer System.” Finally, members will gather at the Dartmouth-Hitchcock Academic Center for a PNHP membership meeting this fall.
To get involved in New Hampshire, please contact Donald Kollisch at Donald.o.kollisch@dartmouth.edu.
New York

In New York, the PNHP NY-Metro chapter joined forces with local health justice advocacy groups, especially retiree groups opposing MA, to celebrate Medicare’s birthday outside Sens. Gillibrand and Schumer’s offices on July 28, 2023. With approximately 70 participants in attendance, activists celebrated with a piñata and cupcakes before attempting to deliver two oversized birthday cards to the legislative offices. This summer, the chapter also had its first in-person fundraising reception since 2019, celebrating their 2023 Single Payer Champions. This year, the chapter honored CIR-SEIU, local business Buunni Coffee, and NY-Metro board member Dr. Marc Lavietes. Approximately 80 people bought tickets, and the reception included live music and a silent auction.
To get involved in the New York metropolitan area, please contact Mandy Strenz at mandy@pnhpnymetro.org.
Eastern Pennsylvania

In Eastern Pennsylvania, chapter members visited Rep. Dwight Evans (D-PA) on the 58th anniversary of Medicare to ask him to cosponsor the Medicare for All bill. The chapter also met with state representative Arvind Venkat, who is also a physician from the Pittsburgh area, to discuss the possibility of proposing a state single-payer bill. On June 3, members gathered at Mt. Airy Day, a major community event in Philadelphia where they collected over 200 postcards for Congressional leaders to support a national single payer bill. These cards were hand-delivered to Senators Casey and Fetterman and Representatives Evans, Scanlon, Houlihan, Dean, and Boyle.
To get involved in Eastern Pennsylvania, please contact Dr. Walter Tsou at macman2@aol.com.
West Virginia
Our chapter in West Virginia continues to grow, and its website went live for the first time in March. Members have been holding regular monthly meetings with speakers on topics such as health care economics, social security, and updates from other state chapters. Efforts continue on membership recruitment at renewal at both state and national levels, as well as national phone banking efforts.
To get involved in West Virginia, please contact Dr. Daniel Doyle at doyledan348@gmail.com.
SNaHP Chapter Reports
Florida State University
SNaHP students at Florida State University have been busy recruiting new members, tabling at student events, and giving presentations. The chapter has also participated in advocacy efforts at the state level through their partnership with the recently consolidated Florida chapter of PNHP. Finally, the chapter has begun collaborating with the SNaHP chapter at the University of Florida, and both chapters are planning to host an event together in the coming year.
To get involved at Florida State University, please contact Xan Nowakowski at xnowakowski@fsu.edu.
Penn State
Students at Penn State have been working hard to prepare for the upcoming school year. The chapter has been working with their Hershey campus counterpart on goals of recruitment and becoming fixtures on their respective campuses. Some of their plans include strategizing around activities fairs, organizing a summer social event to stir conversation around single payer, and putting together a six-part fall seminar series to educate students on the health system and how they can work to fix it with Medicare for All.
To get involved at Penn State, please contact Andrew Meci at ameci@pennstatehealth.psu.edu.
University of Buffalo
At the University of Buffalo, SNaHP students tabled during orientation week for incoming M1 students and had many sign up to be a part of the organization. Members also attended a Community Health Fair at the local Hopewell Baptist Church hosted by the Student National Medical Association; they used this opportunity to go out in the community and educate their neighbors on PNHP’s mission and the benefits of a national healthcare system.
To get involved at the University of Buffalo, please contact Colin Marchincin at cmarchin@buffalo.edu.
University of Minnesota-Twin Cities

The SNaHP chapter at University of Minnesota-Twin Cities co-hosted a viewing and panel discussion of “American Hospitals,” along with Minnesota Nurses Association, PNHP MN, Health Care for all MN, SEIU MN, MN COPAL, and Arts and Medicine UMN. Members met with City Council member Robin Wonsley to request that the Minneapolis City Council create a resolution opposing the merger of hospital systems Fairview Health Services and Sanford Health. The resolution passed unanimously, and the merger was later canceled. Finally, five chapter members participated in PNHP MN’s summer internship program.
To get involved at the University of Minnesota Twin Cities, please contact Sonja Knudson at knuds155@umn.edu.
University of Missouri-Columbia
Students at the University of Missouri-Columbia’s SNaHP chapter organized a monthly repeating voter registration event at their community health clinic for uninsured patients. The chapter also organized a speaking event with PNHP Board Secretary Dr. Ed Weisbart, who spoke to students about reaching across the aisle on discussions around Medicare for All. Finally, members held an educational event for medical students to learn the basics on the Medicare and Medicaid programs.
To get involved at the University of Missouri-Columbia, please contact Lauren Nowakowski at Lmndn9@umsystem.edu.
35th Anniversary House Parties
PNHP National Coordinator Dr. Claudia Fegan and immediate past PNHP President Dr. Susan Rogers hosted a house party in Illinois which was attended by 15 people. Highlights included an engaged discussion on single payer, vegetarian hors d’oeuvres, and homemade sangria! Almost everyone who attended donated, and a lapsed member rejoined PNHP along with making a sizable donation. Drs. Fegan and Rogers also secured 7 new donors, had a new member join, and even inspired an attending couple to host their own event! From a goal of $2000, they raised over $2800.

PNHP Board Member Dr. Eve Shapiro hosted a house party in Arizona along with a co-host. Dr. Shapiro invited people who she knew were interested in the issue of single payer, but not all of them were health professionals. Many invitees came from connections with the local Democratic Party and other progressive activists. Dr. Shapiro felt that having guests invite their own interested friends was key to hosting a successful event, as was encouraging discussion and providing plenty of food and drinks. From a goal of $3500, Dr. Shapiro raised over $4600.
Dr. Nancy Greep hosted a house party in California. She sent out invitations to friends, people who signed PNHP petitions, and neighbors. Dr. Greep invited SNaHP students who really livened up the party and were great at communicating about PNHP with guests. She also prepared a short PowerPoint presentation for guests, which helped to explain PNHP’s mission and what donations would be used for. Overall, Dr. Greep raised $2000.

PNHP member Dr. Leo Alonso hosted a house party in Florida. He invited about 18 friends who shared like-minded views on health care. Dr. Alonso prepared PNHP goodies like stickers and pens, and included a QR code to make on-the-spot donations. After a dinner of homemade pizza and Cuban sandwiches, everyone gathered for a lively and cerebral discussion on Medicare for All, asking questions about how the program would work, common arguments against it, and related issues like fraud in Medicare Advantage.
Dr. Wayne Strouse hosted a house party in New York. Although some of the planned activities couldn’t be carried out due to weather and timing issues, the party was nonetheless successful. Dr. Strouse gave a talk about his experiences living and working in New Zealand, drawing on his experience with the single-payer health care system there to explain what PNHP was working toward in the U.S. The party successfully brought in new donors to PNHP, and raised $1300 on a $500 goal.
Dr. Jessica Schorr Saxe hosted a house party in North Carolina along with Dr. Susan Rucker and Dr. Andrea Desantis. They had food from countries with single-payer, and info by each food station on that country’s particular health system. About 35 people attended from a variety of backgrounds. The hosts spent a few minutes speaking about PNHP and the goals of the fundraising, and then gave a brief ask with the pitch of what PNHP is up against from the investment industry. Several new members and donors came out of the party, and hosts raised over $7600!
PNHP in the News
News items featuring PNHP members
- “Drug costs lead millions in the US to not take medications as prescribed, according to CDC,” CNN, 6/2/23, featuring Dr. Adam Gaffney
- “13 Things You Never Knew You Could Negotiate,” Women.com, 7/17/23, featuring Dr. David Himmelstein
- “Seattle crowd: ‘Medicare for All! Everybody in, nobody out!’,” People’s World, 8/15/23, featuring Bryce Walker
- “Maine Medical Association says American healthcare system needs an overhaul,” Maine Monitor, 9/11/23
- “Insurers Are Gaming Medicare–To The Tune Of $140 Billion,” The Lever, 10/4/23, featuring Dr. Ed Weisbart
- “Medicare Advantage Overbills Taxpayers by $140 Billion a Year—Enough to Wipe Out Medicare Premiums,” Common Dreams, 10/4/23, featuring Dr. Ed Weisbart
- “Physician group slams insurers for overcharging taxpayers for Medicare Advantage,” Medical Economics, 10/10/23
- “There is Too Much Medicare Marketing,” Kiplinger, 10/11/23
Op-eds by PNHP members
- “Health-care workers hamstrung by law denying care to some,” by Dr. A. Joseph Layon, Orlando Sentinel, 7/28/23
- “The Time Has Come for Medicare for All,” by F. Douglas Stephenson, LA Progressive, 7/29/23
- “Just buy it back already,” by Thomas Lane, Minnesota Reformer, 8/11/23
- “Single-payer health care will help solve many problems, not every problem,” by Dr. Samuel Metz, Bend Bulletin, 8/15/23
- “Inside the Big Business of Blood,” by Dr. Adam Gaffney, New Republic, 8/16/23
- “As We See It: SB 1089 establishes governance board to create universal health care plan,” by Dr. Mike Huntingon and Dr. Bruce Thomson, Corvallis Gazette-Times, 8/29/23
- “California Says No to Privatizing Medicare,” by Patty Harvey, North Coast Journal, 9/21/23
- “The Great Medicaid Unwinding,” by Dr. Adam Gaffney, The Nation, 10/6/23
- “Medicare (Dis)Advantage,” by Barry Hermanson, San Francisco Bay View, 10/22/23
- “Medicare Advantage plans may work well for you, until you get sick,” by Dr. Marvin Malek, VTDigger, 10/23/23
Letters to the editor by PNHP members
- “The problem with upcoding under Medicare Advantage,” by Dr. Julie Pease, Portland Press Herald, 8/1/23
- “Make health care work for all,” by Dr. Alan Unell, The Columbian, 9/4/23
- “Save on health care,” by Dr. Henry Abrons, San Francisco Chronicle, 9/7/23
- “Correct income inequality among doctors,” by Dr. George Bohmfalk, Washington Post, 9/8/23
- “We need a single-payer system in the US,” by Dr. Christine Ebert-Santos, Summit Daily, 9/12/23
- “Where do politicians stand on universal care?” by Patty Harvey, Times-Standard, 9/14/23
- “Health care for all,” by Dr. Walter Tsou, Philadelphia Inquirer, 9/26/23
- “Another Reason for Universal Healthcare,” by Dr. Joanne Mallett, Arizona Daily Star, 9/28/23
- “Seniors should avoid Medicare Advantage plans,” by Dr. Ann Troy, Marin Independent Journal, 10/7/23
- “Join Margo in support of ‘Medicare for All’,” by Dr. Michael Marek, Aspen Daily News, 10/9/23
- “Medicare for All our best solution,” by Dr. Tom Jenkins, Chattanooga Times Free Press, 10/14/23
- “Medicare Malady: A second opinion,” by Dr. Ann Troy, Pacific Sun, 10/17/23
- “Protect it,” by Dr. Christine Llewellyn, Virginian-Pilot, 10/20/23
- “It’s Medicare ‘DISadvantage’,” by Dr. Jeff Sklar, Riverdale Press, 10/20/23
- “Politics controls health policy from upstream,” by John Steen, VTDigger, 10/22/23
The post PNHP Newsletter: Fall 2023 appeared first on PNHP.
2023 Annual Meeting 23 Aug 2023 11:22 AM (last year)
Online registration has closed—but onsite registration will be available in Atlanta!
Location
The PNHP Annual Meeting and SNaHP Summit will be held at the Crowne Plaza Atlanta – Midtown, located at 590 W Peachtree St NW, Atlanta, GA 30308.
Sleeping rooms are available at the Crowne Plaza for $169/night and may be booked two ways:
- Online HERE, click “Book Now” and use the group code PNH in the “rate preference” selection.
- Call 404-877-9000 and ask to speak with a reservations agent. Be sure to mention you are booking with the Physicians for a National Health Program group.
Sleeping room reservations must be made by Thursday, Oct. 19.
Schedule of Events
Note changes to the schedule from previous years when planning your travel.
Friday, Nov. 10
- Optional Single Payer and PNHP 101 session, 12:00 p.m.
- Leadership Training, 1:00 p.m. – 5:10 p.m.
- Note: There is no Leadership Training dinner this year
- SNaHP and residents session with CIR, 7:00 p.m. – 8:30 p.m.
Saturday, Nov. 11
- SNaHP welcome session, 8:00 a.m.
- PNHP Annual Meeting, 9:00 a.m. – 5:15 p.m.
- Dedicated SNaHP Summit sessions will be held throughout the day
- Member Interest Group meetings and social hour, 5:15 p.m. – 7:00 p.m.
- PNHP’s 35th Anniversary Dinner, 7:00 p.m. – 9:00 p.m.
Sunday, Nov. 12
- SNaHP Summit, 9:00 a.m. – 12:00 p.m.
- Regional meetings, 9:30 a.m. – 10:30 a.m.
- PNHP Board of Directors meet and greet, 11:00 a.m. – 12:00 p.m.
- Public Action, early afternoon, exact start time and location TBA, expect to finish by 3:00 p.m. – bring your white coat!
To request a meeting for a Member Interest Group (MIG), please contact deputy director Matt Petty at matt@pnhp.org.
This conference will not be livestreamed in its entirety, but recordings of select sessions will be made available after the meeting.
Speakers
 Keynote Speaker: Camara P. Jones, MD, MPH, PhD, “Confronting Racism Denial: Naming Racism and Moving to Action”
Keynote Speaker: Camara P. Jones, MD, MPH, PhD, “Confronting Racism Denial: Naming Racism and Moving to Action”
Dr. Camara Jones is Past President of the American Public Health Association and Commissioner, O’Neill-Lancet Commission on Racism, Structural Discrimination, and Global Health.
 Health Policy Update: Adam Gaffney, MD, MPH and James Waters
Health Policy Update: Adam Gaffney, MD, MPH and James Waters
Dr. Adam Gaffney is Past President of PNHP, assistant professor of medicine at Harvard Medical School, and a pulmonary and critical care physician at Cambridge Health Alliance. James Waters is an executive board member of SNaHP and third-year medical student at Cooper Medical School of Rowan University.
 Messaging Medicare Advantage: Jay Marcellus
Messaging Medicare Advantage: Jay Marcellus
Jay Marcellus is Director of Narrative at ASO Communications, which applies tools from cognition and linguistics to uncover where people are capable of going and how to use our words, images, and stories to move them. ASO has more than a decade’s experience creating, testing, and implementing narratives to achieve progressive wins in the U.S., Australia, and elsewhere.
 Building Progressive Power, Lessons from Georgia: Keron Blair
Building Progressive Power, Lessons from Georgia: Keron Blair
Keron Blair is Chief of Field and Organizing at the New Georgia Project, a nonpartisan effort to register, civically engage, and build power in Georgia for its growing population of Black, brown, young, and other historically marginalized voters.
 Meeting Chair: Philip Verhoef, MD, PhD
Meeting Chair: Philip Verhoef, MD, PhD
Dr. Phil Verhoef is president of PNHP, an adult and pediatric intensivist, and clinical associate professor of medicine at the John A. Burns School of Medicine at the University of Hawaii-Manoa.
Student and Resident Scholarships
Scholarships are available to students and residents to cover a portion of the cost of travel, and for housing in PNHP’s block of student rooms. Apply today HERE; more information is available HERE. Applications are due by August 31.
PNHP members and the public can support PNHP’s student outreach programs by making a GIFT to the Nicholas Skala Student Fund.
Related Action
The Georgia chapter of PNHP is organizing a public action on Sunday, November 12. We will meet at the Martin Luther King, Jr. National Historical Park at 1:00 p.m. and march to the recently closed Atlanta Medical Center for a rally at 1:30 p.m.
PNHP-GA will be joined by national PNHP members, health professionals attending the annual meting of the American Public Health Association, and numerous local health justice organizations to demand full Medicaid expansion in Georgia.
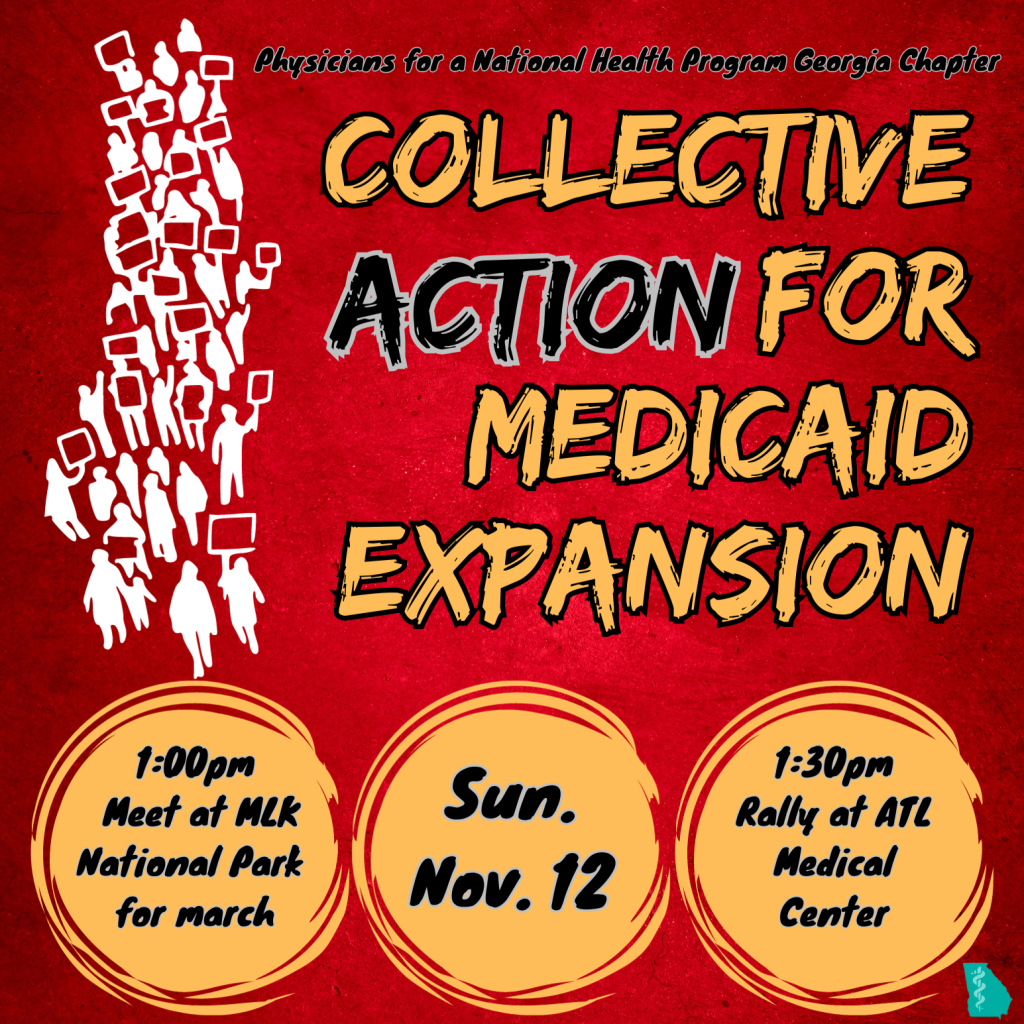
Related Event
The 2023 Health Activist Dinner at APHA will be held on Sunday, Nov. 12, at Paschal’s. Registration and information on honorees will be available soon. PNHP is a co-sponsor of this event.
Covid Safety Protocols
PNHP’s Board of Directors and medical experts have established the following Covid safety protocols for the conference:
- Vaccination requirement within the last 12 months; to ease on-site registration, please email your proof of vaccination to admin@pnhp.org
- Facemasks recommended while not actively eating or drinking

Previous Annual Meetings
Click HERE to access archival material from last year’s Annual Meeting in Boston. Click HERE to view photos from the conference.
Attending the 2023 PNHP Annual Meeting and SNaHP Summit is entirely voluntary and requires attendees to abide by any applicable rules of conduct, or local or state laws, that may be announced at any time. Attendees acknowledge the highly contagious and evolving nature of Covid-19 and voluntarily assume the risk of exposure to, or infection with, the virus by attending the Meeting, and understand that such exposure or infection may result in personal injury, illness, disability, and/or death. Attendees release and agree not to sue any persons or entities responsible for coordinating or organizing the PNHP Annual Meeting and SNaHP Summit in the event that they contract Covid-19. Attendees agree to comply with all Covid-related procedures that may be implemented at the Meeting, including mask-wearing.
The post 2023 Annual Meeting appeared first on PNHP.
Kitchen Table Campaign: Medicare Disadvantage 25 Jul 2023 9:49 AM (last year)
PNHP is committed to focusing on specific “Kitchen Table” issues, to show how single-payer Medicare for All would address Americans’ most pressing health care problems. See below for materials related to our Summer 2023 issue, the so-called “Medicare Advantage” program, and scroll to the bottom for a list of additional topics.

Medicare Disadvantage (Summer 2023)
What happened when policymakers invited big insurance companies like Cigna and UnitedHealthcare to administer Medicare benefits? Nothing good. These companies followed the same old script: restricting seniors’ choice of doctor, delaying or denying medically necessary care, and laughing all the way to the bank.
We encourage you to share the materials below with your colleagues, family members, friends, and neighbors during the summer of 2023 to remind them that the growth of Medicare Advantage is a kitchen table issue…and that Medicare for All would deliver better coverage, more meaningful choices, and true financial freedom.
Learn more about Medicare Advantage
- One-pager: Medicare Advantage; Bad for Patients, Great for Profiteers
- Policy primer: The Problems with Medicare Advantage
- Comparison chart: Medicare Advantage vs. Medicare for All
- PNHP comment: CMS Should Terminate the Medicare Advantage Program
- PowerPoint slides: Don’t Let Naked Profiteering Destroy our Medicare
Raise the alarm about Medicare profiteering by writing an op-ed or letter to the editor. Looking for tips on getting published? Email PNHP communications specialist Gaurav Kalwani at gaurav@pnhp.org.
PNHP report on Medicare Advantage overpayments
In the fall of 2023, PNHP published a report detailing the many ways that so-called “Medicare Advantage” plans overcharge taxpayers. We found that total overpayments amount to at least $88 billion, and potentially up to $140 billion, each and every year.
By simply eliminating these excess payments, we could fund valuable improvements to the Traditional Medicare program, such as eliminating Part B premiums altogether or adding comprehensive dental, vision, and hearing benefits.
Dr. Ed Weisbart: Don’t let naked profiteering destroy our Medicare
Presented by PNHP national board secretary Dr. Ed Weisbart to members of Puget Sound Advocates for Retirement Action (PSARA) on March 20, 2023. PowerPoint slides available HERE.
Survey for physicians and Medicare beneficiaries
- Short survey for Medicare beneficiaries (online and print versions)
- Short survey for physicians (online and print versions)
- One-page fact sheet to accompany the survey
- Medicare Advantage petition, available at pnhp.org/MAPetition
We urge our members and chapters to distribute these surveys at public events! Questions? Email PNHP national organizer Lori Clark at lori@pnhp.org.
Day of action in Washington, D.C.
PNHP was proud to join our friends at Be a Hero, Social Security Works, Public Citizen, and National Nurses United—along with dozens of New York City retirees, legislative champions, and patients affected by Medicare Advantage—for a DC Day of Action on July 25, 2023.
Host a house party in support of our MA campaign
- Complete house party planning guide, including FAQs, a checklist, and a sample house party agenda
- Complete house party communications guide, including sample language for emails, texts, voicemails, and social media posts
- Set up your very own personal fundraising page to fight Medicare privatization
Fighting profiteering in the Medicare program is one of the main priorities of PNHP’s 35th anniversary campaign. Questions? Email PNHP national organizer Lori Clark at lori@pnhp.org.
Social media materials
Download our series of eight (8) “scam alert” graphics HERE, and an additional Medicare Advantage meme HERE. Questions about social media? Email PNHP communications specialist Dixon Galvez-Searle at dixon@pnhp.org.
Additional topics
Review previous installments of the Kitchen Table Campaign, and stay tuned for additional topics in the future:
- Surprise billing (January 2020)
- Racial health inequities (February 2020)
- Rural health (March 2020)
- Pandemics and public health emergencies (April 2020)
- COVID-19 and racial health inequities (Spring 2020)
- COVID-19 endangers health care workers (Summer 2020)
- Measuring candidate health plans (Fall 2020)
- Mental health care (Spring 2021)
- Maternal mortality (Summer 2021)
The post Kitchen Table Campaign: Medicare Disadvantage appeared first on PNHP.